
Frailty, Inflammation, and Waitlist Mortality among Patients with End-Stage Renal Disease on the Kidney Transplant Waitlist
Mara McAdams DeMarco1, Hao Ying1, Alvin Thomas1, Fatima Warsame1, Ashton Shaffer1, Christine Haugen1, Jacqueline Garonzik-Wang1, Niraj Desai1, Ravi Varadhan1, Jeremy Walston1, Silas Norman2, Dorry Segev1.
1Johns Hopkins, Baltimore, MD, United States; 2University of Michigan, Ann Arbor, MI, United States
Background: Among community-dwelling older adults, frailty is associated with heightened inflammation and subsequent mortality. Although frailty is common among patients on the KT waitlist, the role of frailty and inflammation in this population remains unclear. We quantified the association between frailty, inflammation, and mortality in ESRD patients on the KT waitlist, and tested whether frailty and/or inflammation improves risk prediction beyond clinical factors available in registry-based models.
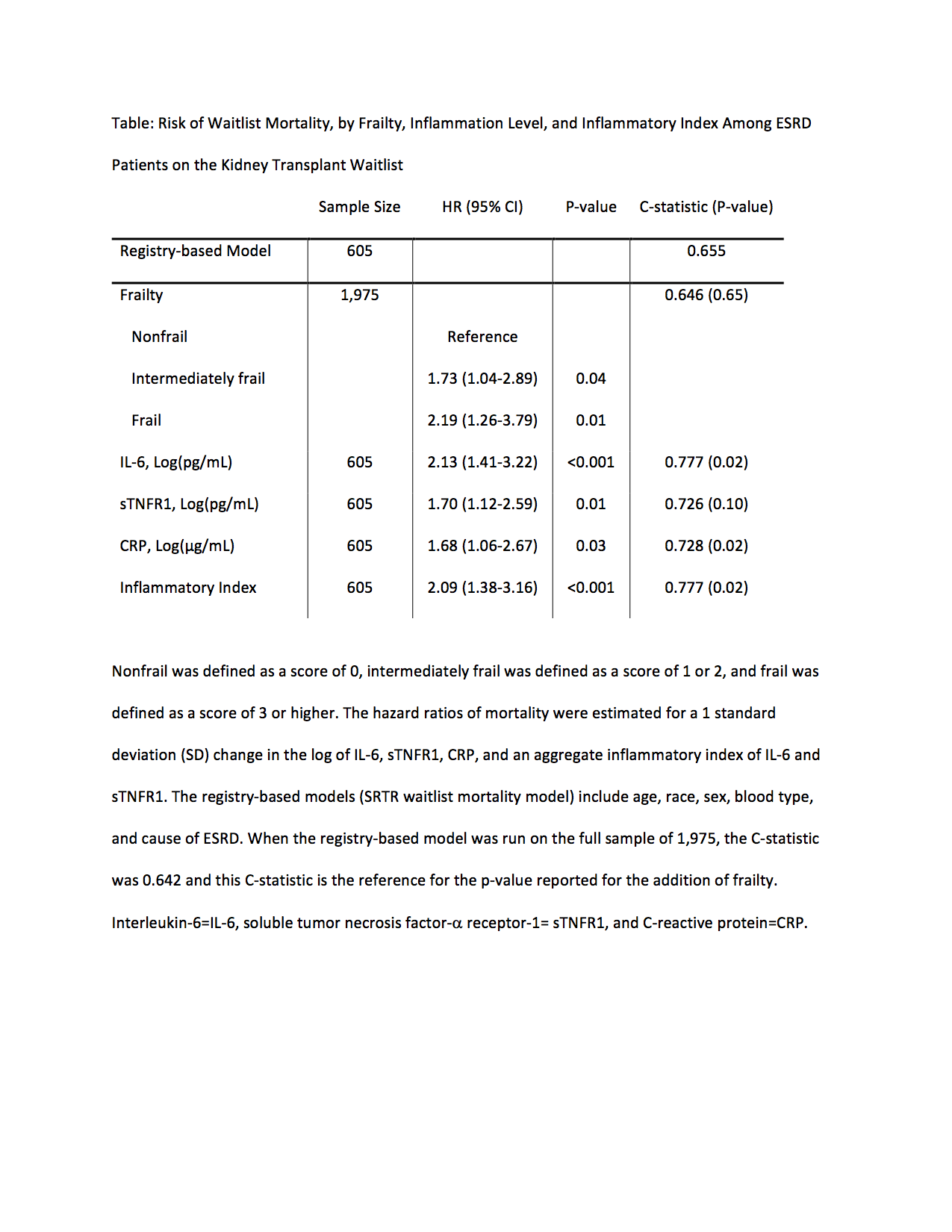
Methods: We studied 1,975 prevalent ESRD patients on the KT waitlist (11/1/09-2/28/17) in a multi-center cohort study of measured frailty in patients undergoing transplant evaluation; serum inflammatory markers (interleukin-6 [IL-6], soluble tumor necrosis factor-a receptor-1 [sTNFR1], and C-reactive protein [CRP]) were analyzed in 605 of these participants. We compared the C-statistic of an established registry-based prediction model adding frailty and/or inflammation (1SD change in log IL-6, sTNFR1, CRP, or an aggregate inflammatory index).
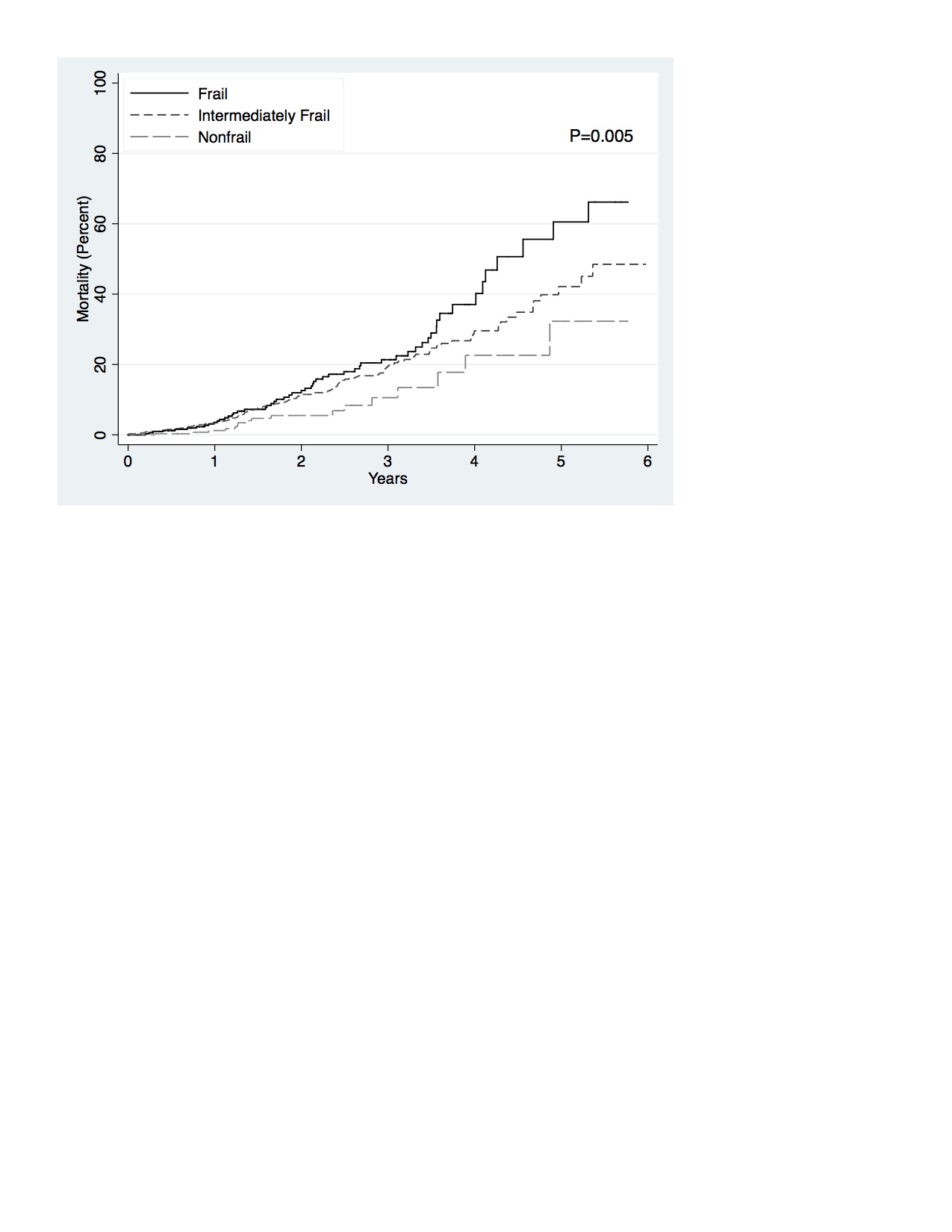
Results: The mean age was 53.7 and 18.4% were frail. Frail candidates had elevated serum IL-6 (P<0.001), sTNFR1 (P=0.02), CRP (P=0.01), and a higher inflammatory index (P<0.001). The registry-based model had moderate predictive ability (C-statistic=0.655). Frailty was associated with increased waitlist mortality risk (frail HR=2.19, 95%CI:1.26-3.79) (Figure) but did not improve mortality risk prediction (C-statistic=0.646; P=0.65) (Table). Like frailty, IL-6 (HR=2.13, 95%CI:1.41-3.22), sTNFR1 (HR=1.70, 95%CI:1.12-2.59), CRP (HR=1.68, 95%CI:1.06-2.67), and the inflammatory index (HR=2.09, 95%CI:1.38-3.16) were all associated with increased waitlist mortality risk. But unlike frailty, adding IL-6 (C-statistic=0.777; P=0.02), CRP (C-statistic=0.728; P=0.02), or the inflammatory index (C-statistic=0.777; P=0.02) substantially improved mortality risk prediction.
Conclusions: Among adult ESRD patients on the KT waitlist, frailty and inflammation were associated with increased waitlist mortality risk, but only inflammatory markers significantly improved mortality risk prediction. Heightened inflammation may be the biological link between frailty and mortality in KT candidates.
This study was supported by NIH grant R01AG042504 (PI: Dorry Segev), R01AG055781 (PI: McAdams-DeMarco) and K24DK101828 (PI: Dorry Segev). Mara McAdams-DeMarco was also supported by the Johns Hopkins University Claude D. Pepper Older Americans Independence Center (P30AG021334), National Institute on Aging (K01AG043501). Christine Haugen was supported by the National Institute on Aging (F32AG053025). Ashton Shaffer was supported by the National Institute of General Medical Sciences (5T32GM007309)..
