Pancreas Graft Outcomes in Living versus Deceased Kidney Donor in Pancreas after Kidney Transplant Recipients
Pedro Ventura-Aguiar1, Joana Ferrer2, Ignacio Revuelta1, David Paredes3, Erika De Sousa-Amorim1, Jordi Rovira1, Enric Esmatjes4, Juan Carlos Garcia-Valdecasas2, Federico Oppenheimer1, Fritz Diekmann1, Maria Jose Ricart1.
1Nephrology and Kidney Transplant Department, Hospital Clinic, Barcelona, Spain; 2Hepatobiliopancreatic and Liver Transplant Department, Hospital Clinic, Barcelona, Spain; 3Organ Transplantation Coordination Department, Hospital Clinic, Barcelona, Spain; 4Diabetes Unit, Department of Endocrinology and Nutrition, Hospital Clinic, Barcelona, Spain
Introduction: The advantages presented by pancreas after kidney transplantation (PAK) are often outweighed by conflicting results as to patient and pancreas graft survivals’, when compared to simultaneous kidney-pancreas (SPK). Immunological factors, such as shared mismatches, or kidney transplant donor (living- or deceased-donor) may play a role in these outcomes.
Methods: We retrospective analyzed all pancreas transplants performed at our center since the beginning of the pancreas after living-donor kidney transplantation (PAldK) program in 2007, and compared patient and grafts survivals’, and acute rejection incidence between PAldK (n=18), SPK (n=139) and pancreas after deceased kidney transplant (PAddK; n=28).
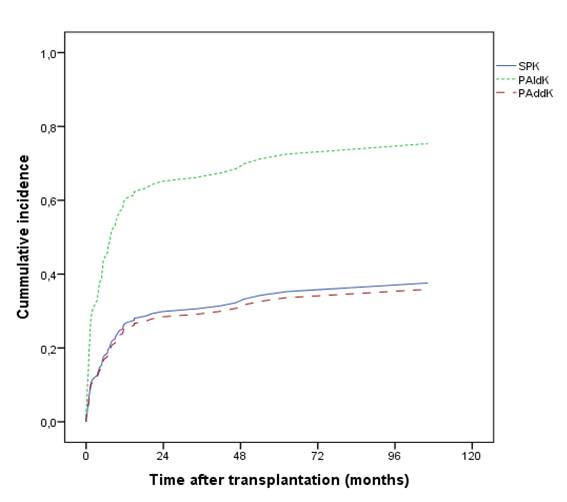
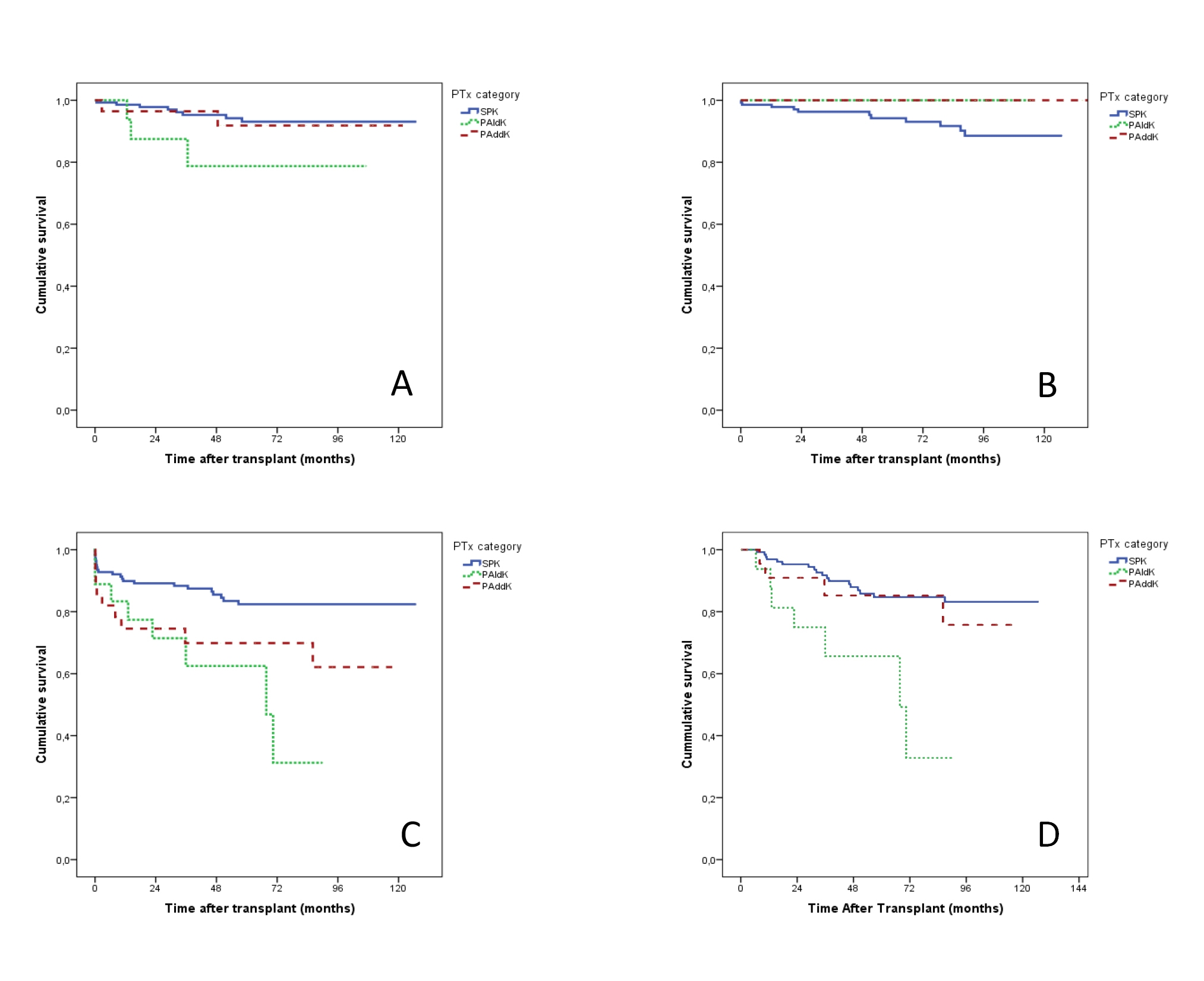
Results: Overall patient, kidney, and pancreas grafts survivals’ (death-censured) at 12 months was 98%, 99%, and 86%, respectively, and at 5 years 93%, 96%, and 80%. Kaplan-Meier pancreas graft survival estimates were similar between the three groups, but inferior for PAldK when included only those with functioning pancreas at day 90 post-transplant (log-rank p=.004). In a binary logistic regression, both PAK groups presented an increased risk for pancreas graft failure (PAldK HR 3.58 95% CI 1,59-8,08; PAddK HR 2,30 95% CI 1,06-5,00; p<.05).
Pancreas acute rejection was significantly increased in PAldK (67%; 1,8±1,4 episodes/graft) when compared to PAddK (25%) and SPK (32%) (p<.05). In a multivariate Cox regression model including known risk factors for pancreas rejection, PAldK was the only factor associated with an increased risk for rejection (HR 6,82 95% CI 1,51-30,70, p<.05). No association was found between pancreas donor-recipient HLA mismatches and graft rejection. In both PAK groups, shared HLA incompatibilities between kidney and pancreas donors (0 vs 1-6) didn’t correlate with pancreas graft rejection or survival (p>.05).
Conclusion: PAldK transplant was associated with worst pancreas graft outcomes when compared to PAddK and SPK, but with similar patient and kidney survival. It may be advisable to centers to individually evaluate their median waiting-list time before proposing this alternative to patients.