Outcomes from Livers Transplanted from Deceased Donors with End-Stage Renal Disease
Marty Sellers1,2, Paula Lawrence1, David Marshman1, Kathleen Lilly1, Jean Davis1, Lee Langley1.
1LifeLink of Georgia, LifeLink Foundation, Norcross, GA, United States; 2Surgery, Emory University, Atlanta, GA, United States
Introduction: Decedents with end-stage renal disease (ESRD) have comorbidities that also impact the quality of extra-renal, especially thoracic, organs. Livers, however, are less susceptible to ESRD-associated damage, yet many organ procurement organizations (OPOs) in the United States have not pursued such donors because of financial and regulatory disincentives. Because of the high liver waitlist mortality, however, all usable livers should be transplanted. No data are published on the outcomes of livers transplanted from deceased donors with ESRD; if outcomes are acceptable, financial disincentives must be addressed. We describe the outcomes of livers retrieved from donors with ESRD in a single OPO.
Methods: Donors (n=47) with ESRD who donated livers from January 2010-May 2017 were identified in a prospective database; relevant variables were extracted into a separate database analyzed with Stata. Our primary aim was to determine graft and patient survival; these data were obtained from TEIDI and from the transplant centers.
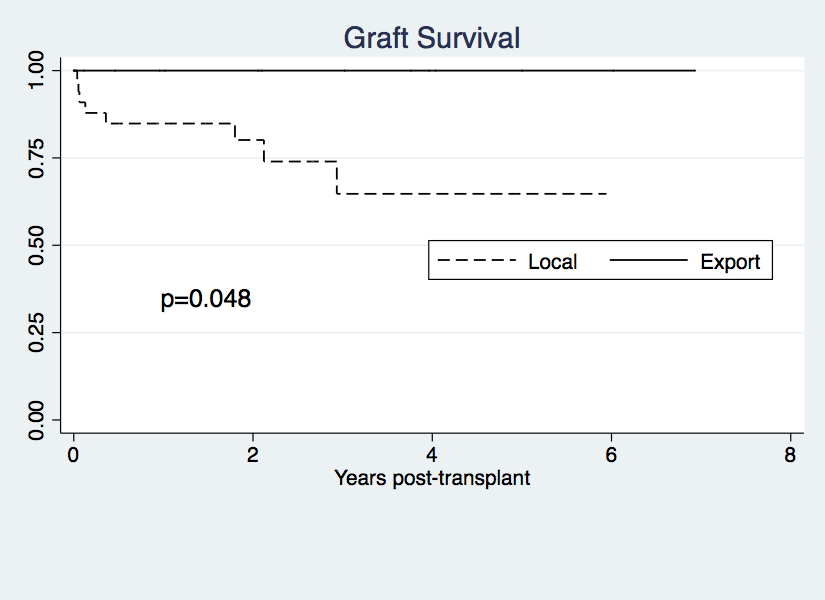
Results: 47 livers were retrieved and transplanted from ESRD donors. Mean time on dialysis was 3.3 years (range 1 month to 13 years). Causes of death included CVA (n=24), anoxia (n=19), trauma (n=3), other (n=1). Two recipients died within 30 days (hemorrhage, day 19; multisystem organ failure, day 23); one patient was retransplanted on day 14 (unknown cause of graft loss). All other patients (95.8%) and grafts (93.6%) survived more than 30 days (Figure 1). Interestingly, livers exported out of our service area (n=14) had significantly better survival than those transplanted locally (Figure 2). No other variable analyzed impacted graft survival. Ischemic times ranged from 2.2 to 10. 6 (mean = 6.0) hours were similar between exported and locally transplanted livers – mean = 6.4 and 5.9 hours, respectively, p=0.813.
Conclusions: Livers from donors with ESRD can be transplanted with excellent outcomes, especially in circumstances where short ischemic times can be achieved. Given the high liver waitlist mortality worldwide, these donors should be aggressively pursued. Financial and regulatory disincentives must be eliminated in order to increase the number of livers retrieved and transplanted.