Does Acute Kidney Injury Contraindicate Transplantation of Kidneys from very Small Pediatric Donors? Single-center Analysis of 68 en Bloc Kidney Transplants from Donors ≤15 kg
Christoph Troppmann1, Chandrasekar Santhanakrishnan1, Kathrin Troppmann1, Ghaneh Fananapazir2, Richard Perez1.
1Department of Surgery, University of California, Davis School of Medicine, Sacramento, CA, United States; 2Department of Radiology, University of California, Davis School of Medicine, Sacramento, CA, United States
Background: Kidneys from very small pediatric donors that have acute kidney injury (AKI) are frequently discarded due to concerns about the potentially negative effects of the AKI on short- and long-term outcomes. We tested the hypothesis that AKI does not adversely impact outcomes of en bloc kidney grafts from very small donors.
Patients and Methods: We defined AKI as terminal donor creatinine [mg/dL] ≥1.5 for donors 0-14 days old and ≥1.0 for donors >14 days old. Among 219 pediatric en bloc kidney transplants from donors ≤15 kg performed 11/2003-01/2015 at our institution, we identified 29 AKI grafts and pair-matched these (for donor weight, DCD setting [7%], and preservation time) with 29 no-AKI grafts (median overall recipient age, 50.3 [7-76] years). Our standard management protocol for en bloc grafts includes hypothermic pulsatile perfusion pre-implantation, rATG induction, and steroid-free maintenance with tacrolimus and mycophenolate mofetil.
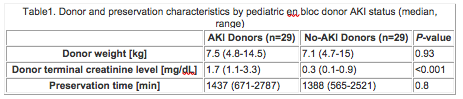
Results: Donor and preservation characteristics are given in Table 1.
Delayed graft function (dialysis during the first week posttransplant) was more frequent in AKI (48%) vs. no-AKI (14%) grafts (p=0.01). Early graft loss from graft thrombosis or primary non-function occurred for 3 (10%) AKI vs. 2 (7%) no-AKI grafts (p=n.s.).
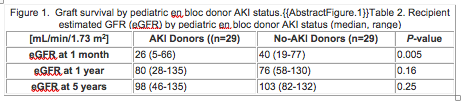
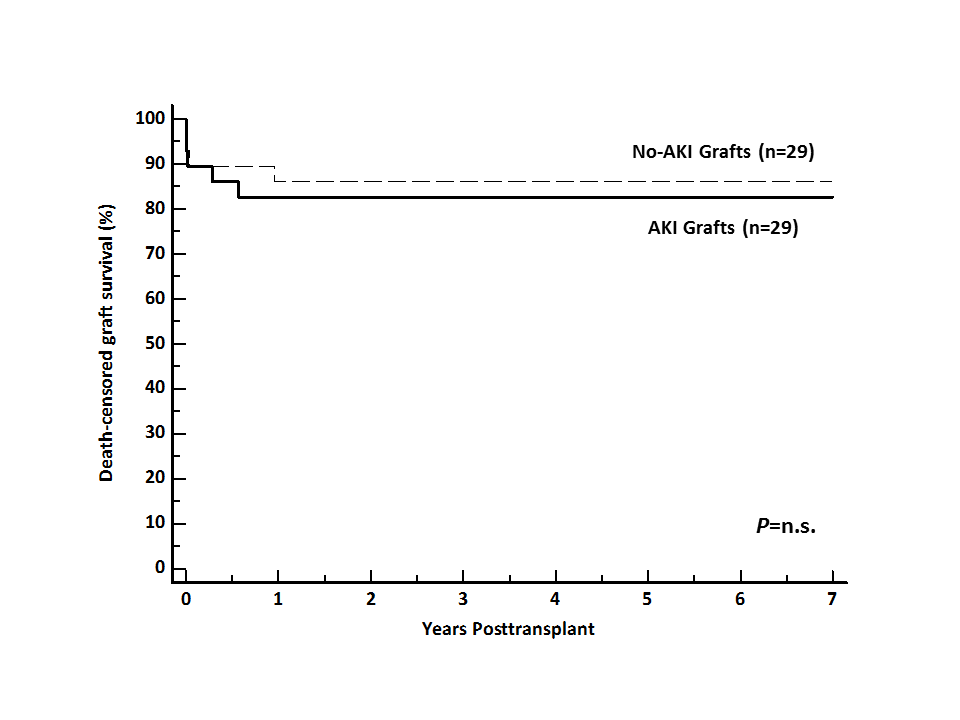
At 1 and 5 years, neither death-censored graft survival (Figure 1) nor graft function (Table 2) were significantly affected by donor AKI.
Conclusions: Despite the slower early function in the AKI group, long-term survival and function of en bloc grafts from small (≤15 kg) donors were were not impacted by donor AKI. Our outcomes suggest (i) that AKI in small pediatric donors should not be viewed as a contraindication to organ donation and (ii) that these donors can effectively expand the limited deceased organ donor pool.
