
Tuberculosis in Living Donor Kidney Transplant Recipients
Mukunda Kafle1, Mahesh Raj Sigdel1, Midhan Shrestha1, Rabin Nepali1, Santosh Chhetri1, Dibya Singh Shah1.
1Department of Nephrology, Tribhuvan University Teaching Hospital, Institute of Medicine, Kathmandu, Nepal
Introduction: Infection with Mycobacterium tuberculosis is a major public health issue in the developing world. Immunosuppressed patients are at high risk of acquiring new infection whilst being equally at risk for reactivation of an indolent disease. Because tuberculosis (TB) can affect any organ system, and even typical infections may present atypically in the immunosuppressed, clinical diagnosis of TB is not easy. Rifampicin based treatment is further challenging because of its interactions with calcineurine inhibitors, an integral component of post-transplant medication. We aimed to study the burden, clinical characteristics and outcome of TB in this setting.
Materials and Methods: This is a retrospective review of follow up of patients who underwent living donor kidney transplantation in our hospital from 8 Aug 2008 to 16 July 2014. Their demographic data, status of post-transplant renal function, rejection and infections were recorded in Microsoft Excel®. Other variables recorded for patients diagnosed to have TB were: time since transplant, type of TB, diagnostic method, treatment regimen, difference in tacrolimus dose before and at the end of rifampicin use, difference in serum creatinine after treatment, and outcome.
Results: Total 250 patients underwent kidney transplant during the period. Mean age was (35.63±10.9) years and male to female ratio was 4.2:1. Data from 26 (10.4%) of these were missing.
Total 15 (6.7%) patients were diagnosed as TB and were prescribed anti tubercular treatment. Median time since transplant till the diagnosis of TB was 182 (range 1-380) weeks.
Majority of patients were diagnosed to have abdominal TB (n=7, 46.67%).(Figure 1) 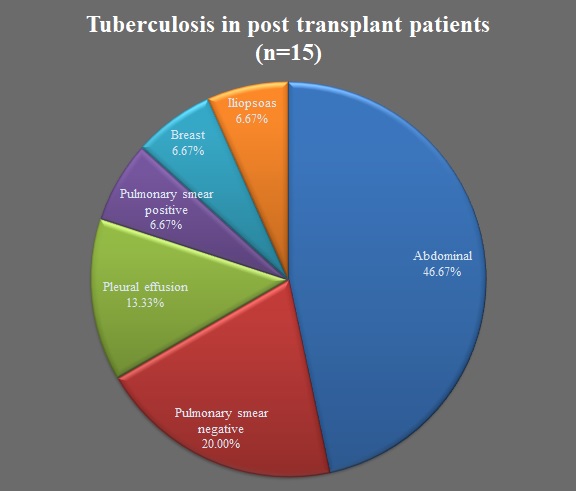
Diagnosis of intestinal and peritoneal TB is difficult. So, the commonest approach was empirical therapy. Constitutional symptoms and unexplained weight loss was the most common (n=6) diagnostic strategy.(Figure 2)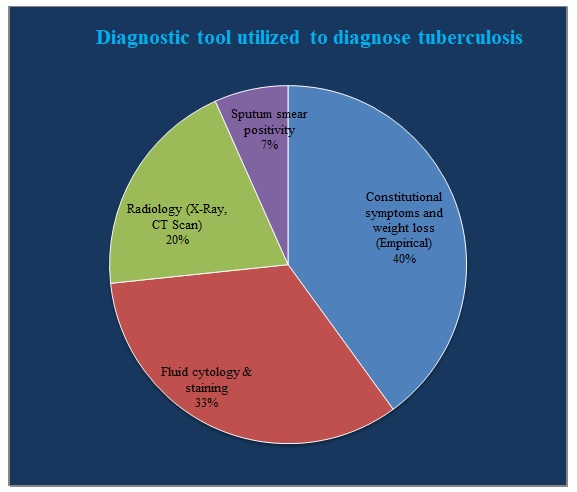
All patients were treated in two (intensive and continuation) phases. Duration of each phase was variable and the most commonly utilized regimen was 2HRZE + 6HR (n=6). Rifampicin was used in 14 (93.33%) patients.
All received induction; daclizumab in 5 and rATG in10. One patient was sensitized and had undergone pre and post transplant plasma exchange. Of the 15 patients, 4 were treated for suspected rejection beforehand, only 3 having biopsy proven rejections (2 ACR, 1 AbMR). Average increment in tacrolimus dose was by 143% (range 0-350%).
As of 2017 December, 2 patients died, 2 lost to follow up, 1 developed graft dysfunction due to noncompliance and 10 have good graft function. Mean change in serum creatinine was -4.30 µmol/L after the treatment. One death occurred during treatment of TB and another patient died with a functioning graft 16 months after the treatment was over.
Conclusions: Diagnosis and treatment of tuberculosis in post-transplant patients is challenging.
Keywords: Tuberculosis, Pleural effusion, Rifampicin, Tacrolimus, Weight loss
