
MHC-Matched A-Expressing Blood Cells Induce ABO Tolerance in Infant and Adult Mice
Bruce Motyka1,2, Jordana Fersovich1, Brendon Lamarche1, Morgan Sosniuk1, Ibrahim Adam1,2, Jean Pearcey1,2, Kesheng Tao1,2, Christopher W Cairo3,4, Peter J Cowan5, Lori J West1,2,4,6.
1Dept. Pediatrics, Alberta Transplant Institute, University of Alberta, Edmonton, AB, Canada; 2Canadian National Transplant Research Institute, University of Alberta, Edmonton, AB, Canada; 3Dept. Chemistry, University of Alberta, Edmonton, AB, Canada; 4Alberta Glycomics Centre, Canadian Glycomics Network, University of Alberta, Edmonton, AB, Canada; 5Immunology Research Centre, St Vincent’s Hospital, Melbourne, Australia; 6Depts. Medical Microbiology & Immunology, Surgery, and Laboratory Medicine & Pathology, University of Alberta, Edmonton, AB, Canada
Purpose: ABO-incompatible heart transplantation (ABOi HTx) is safe during infancy and allows increased donor access. Post-ABOi HTx B cell tolerance develops to donor blood group antigen(s) by mechanisms not fully defined. We developed A-transgenic mice (A-Tg) that express A-antigen on vascular endothelium and erythrocytes and demonstrated A-antigen specific tolerance induced by HTx into 4 wk-old, MHC-identical, wild-type (WT) mice. Herein, we explored intentional tolerance induction in infant and adult WT mice using A-Tg blood cells.
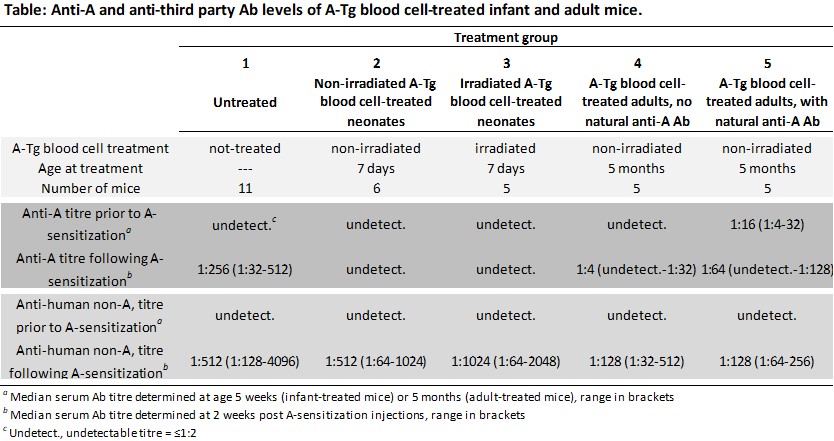
Methods: WT BALB/c mice were injected ip (weekly×3) with intact A-Tg BALB/c blood cells (±40Gy irradiated), beginning at 7 days (neonates) or 5 months of age (adults; see Table). Two weeks after treatment, all mice were injected ip (weekly×5) with human A-erythrocytes (‘A-sensitized’) in an attempt to elicit anti-A antibody (Ab) production. Serum anti-A and 3rd-party (non-A anti-human) Ab were assessed by hemagglutination assay.
Results: In response to A-sensitization, high levels of anti-A Ab were produced in untreated mice (group 1, Table). In contrast, anti-A remained undetectable in A-sensitized mice previously treated as neonates with A-Tg blood cells ±irradiation (groups 2&3). Treatment of adult mice (groups 4&5) with A-Tg blood cells resulted in reduced anti-A production in response to A-sensitization compared with untreated mice (group 1). Adult mice with undetectable natural anti-A (group 4) produced less anti-A vs those with pre-existing natural anti-A (group 5). Third-party antibody responses were high for all groups.
Conclusions: Our results suggest that the erythrocyte component of A-Tg blood cells can induce robust A-antigen-specific tolerance in WT mice. Importantly, our findings suggest that tolerance to A-antigen is not limited to the neonatal period but can also be induced in adults, especially in mice without previously detectable natural anti-A antibody. Intentional induction of tolerance to A/B-antigen(s) may allow subsequent ABOi HTx.
Supported by Heart and Stroke Foundation of Canada; Women and Children’s Health Research Institute, University of Alberta; Alberta Innovates Health Solutions; and the Canadian Institutes of Health Research (CIHR) through the Canadian National Transplant Research Program (CNTRP).
