Helper Innate Lymphoid Cells (hILC) resist Immunosuppressive Therapy: an Observation from Kidney and Liver Transplantation
Elena Gómez Massa 1,2, Paloma Talayero1,2, Alberto Utrero2, Rocío Laguna2, Amado Andrés3, Pilar Auñón3, Ángel Sevillano3, Esther Mancebo1,2, María José Castro1, Estela Paz1,2.
1Immunology, Hospital Universitario 12 de Octubre, Madrid, Spain; 2Instituto de Investigación , Hospital Universitario 12 de Octubre, Madrid, Spain; 3Nephrology, Hospital Universitario 12 de Octubre, Madrid, Spain
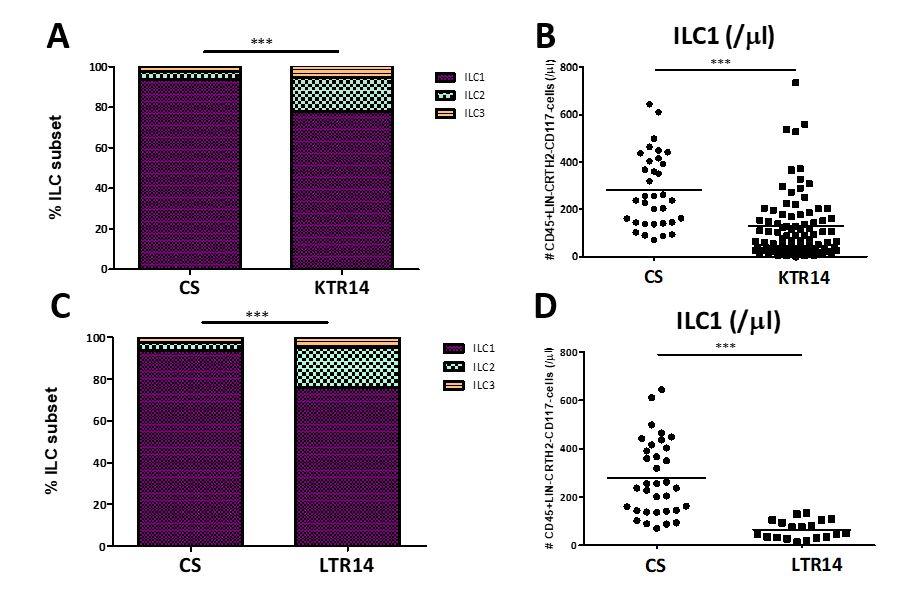
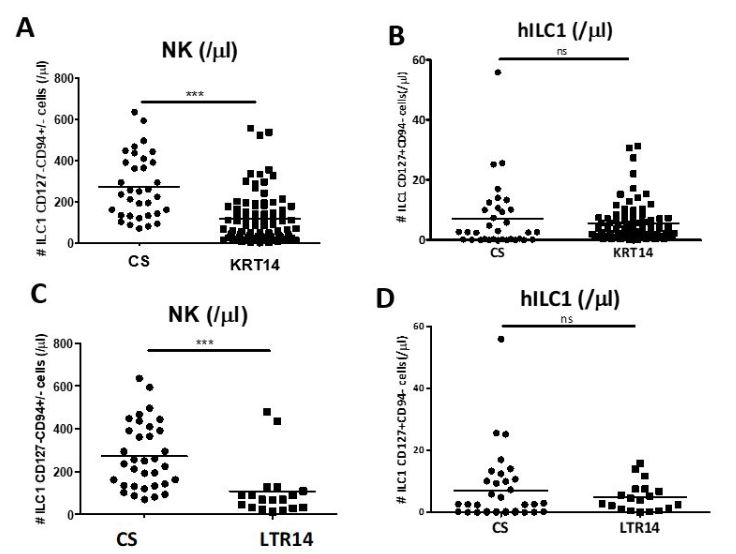
Introduction: We have previously observed that CD3+ CD8+ lymphocytes are depleted in the graft epithelium of intestinal transplant recipients who receive immunosuppressive therapy, while innate lymphoid cells type 1 and 3 (ILC1 and ILC3) persist in high proportions. In this study we compare the ILC representation and its subsets (ILC1, including NK and non-cytotoxic helper ILC1 cells (hILC1), ILC2 and ILC3) in peripheral blood of kidney and liver transplanted recipients versus control subjects (CS) in order to identify possible frequency variations in the context of immune alloresponse and immunosuppressive therapy (IT).
Materials and Methods: Peripheral blood mononuclear cells (PBMCs) were obtained at day +14, from 88 kidney recipients (KTR14): 11 received only triple therapy (No-I), 46 received induction therapy with thymoglobulin (I-TMG) and 31 with Basiliximab (I-Bas), from 19 liver recipients (LTR14): 16 were No-I and 3 I-Bas) and from 48 CS. Total ILC were identified by flow cytometry as CD45+ Lin- (CD3, CD19, CD14) and its subsets were defined as: ILC1 (CD117-CRTH2-), ILC2 (CD117-CRTH2+) and ILC3 (CD117+ CRTH2-). ILC1 were subdivided in NK and hILC1 according to CD127 and CD94.
Results and Discussion:
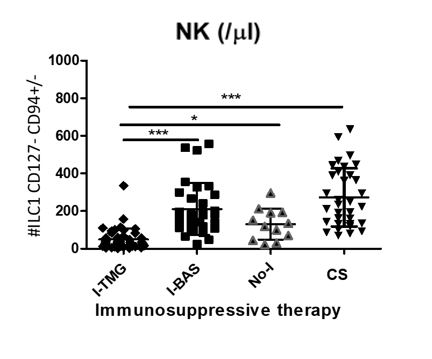
Conclusion: hILC are unaffected by TMG and Basiliximab used as induction therapy for kidney and liver transplantation. hILC are also unaffected by tacrolimus-based triple therapy used as maintenance treatment.
