Revascularization Time Matters in Liver Transplantation: Prolonged Implantation of Marginal Grafts Independently Predicts Inferior Transplant Outcomes in the Short and Long Term
Bettina M Buchholz1, Undine A Gerlach1,3, Vishnu V Chandrabalan1, James Hodson2, Bridget Gunson1, Hynek Mergental1, Paolo Muiesan1, John R Isaac1, Keith J Roberts1, Darius F Mirza1, M Thamara PR Perera1.
1Liver Unit, Queen Elizabeth Hospital Birmingham, Birmingham, United Kingdom; 2Department of Medical Statistics, Institute of Translational Medicine, University Hospitals Birmingham NHS Foundation Trust , Birmingham, United Kingdom; 3Department of General, Visceral and Transplantation Surgery, Charite Universitaetsmedizin Berlin, Campus Virchow Klinikum, Berlin, Germany
Background: In the era of marginal organ utilization, the impact of revascularization time (RT) on outcomes in liver transplantation (LT) has not been reported.
Methods: All primary LT performed in Birmingham between 2009 and 2014 (n=678) with portal reperfusion first were stratified according to RT (<44 vs. ≥44 min) and graft quality (SLG, Donor risk index [DRI]<2.3 vs. MLG, DRI≥2.3).
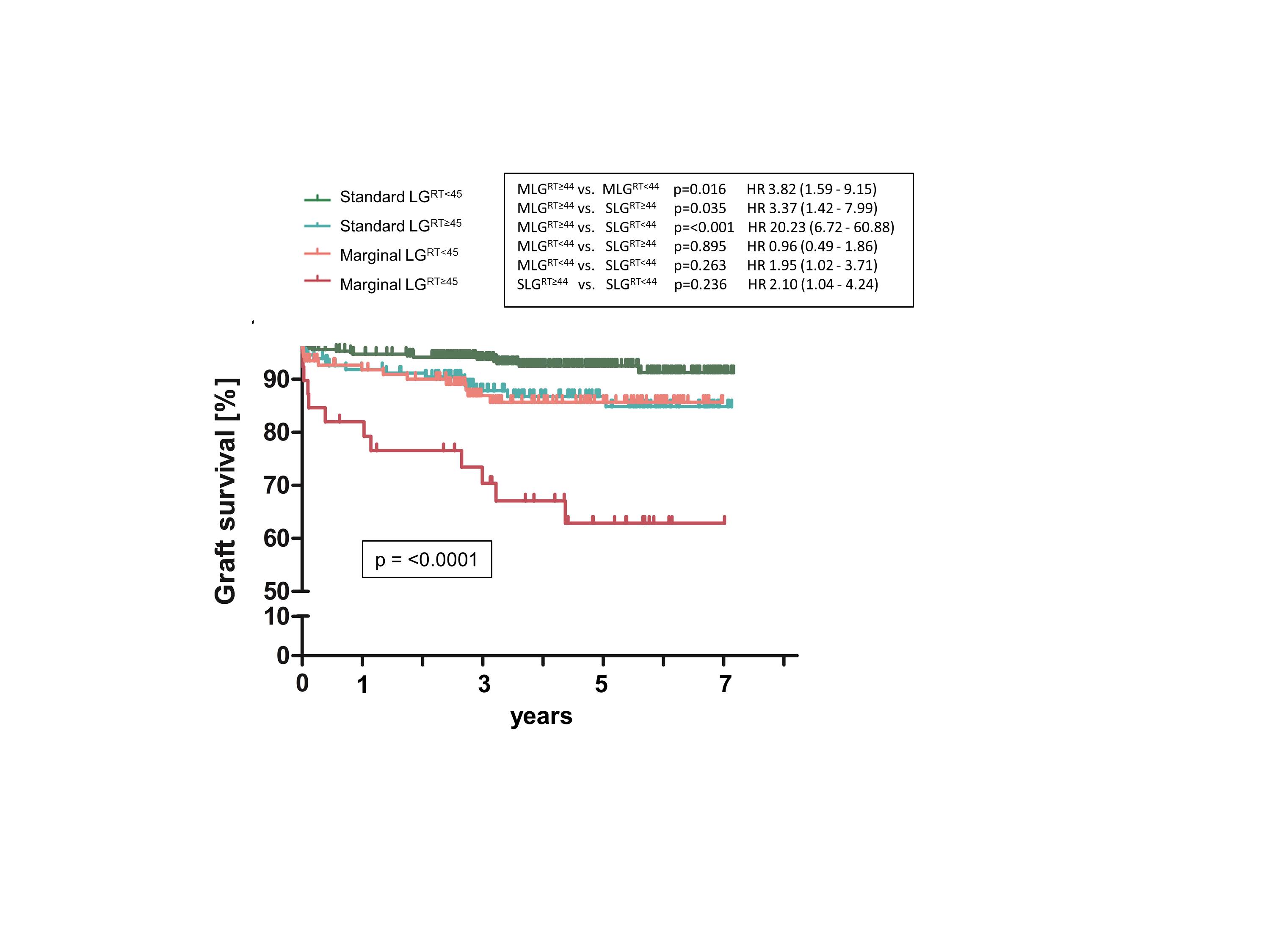
Results: Compared to RT<44, a significantly greater incidence of early allograft dysfunction (EAD) (29% vs. 47%, p=<0.001), post-transplant acute kidney injury (AKI) (39% vs. 60%, p=<0.001) and new-onset AKI after LT (37% vs. 56%, p=<0.001) occurred after RT≥44. RT≥44 was also associated with adverse long-term outcome (3-year graft survival 92% vs. 83%, p=0.001; 3-year patient survival 87% vs. 79%, p=0.004). RT≥44 independently predicted EAD, renal dysfunction and overall graft but not patient survival. The cumulative effect of prolonged revascularization in marginal grafts (MLGRT≥44) resulted in the worst transplant outcome compared to all other groups which could be mitigated by rapid revascularization (SLGRT<44, SLGRT≥44, MLGRT<44 vs. MLGRT≥44, EAD 24%, 39%, 39% vs. 69%, respectively; p=<0.001 and 3-year graft survival 94%, 87%, 88% vs. 70%, respectively; p=<0.001) (Figure 1).Conclusions: Prolonged graft revascularization places outcomes particularly of marginal liver grafts at risk, and this is a modifiable variable that relies on the expertise of the implanting surgeon and also has implications for transplant surgical training.