Evaluate the Efficacy of Epidural Dexmeditomidine as Postoperative Analgesic in Live Donor Renal Allograft Recipients for Open renal Transplantation Surgical Approach
Geeta Parikh1, Bina P. Butala1, Manisha P. Modi1, Tanu P. Mehta1, Krunal A. Patel1, Veena R. Shah1.
1Department of Anesthesiology and Critical Care, Institute of Kidney Diseases and Research Centre and Institute of Transplantation Sciences , Ahmedabad, India
Introduction: Efforts to find better adjuvant in regional anesthesia are underway since long. Dexmedetomidine is a new alpha-2 adrenergic agonist with an ability to provide postoperative analgesia. Our aim was to assess the efficacy of Dexmedetomidine as an analgesic through epidural route with special emphasis on its sedative property and other side effects.
Methods and materials: A prospective randomized double blinded study was carried out with informed written consent after Institutional Review Board approval from June, 2016 to October, 2017; in 60 volunteer patients suffering from end stage renal diseases and posted for open renal transplantation. ASA physical status III and IV were randomly divided into two groups. Group-I (G1) was Levobupivacaine + Dexmedetomidine (LD) and Group-II (G2) was only Levobupivacaine (L). Each group had 30 patients. Injection (Inj.) Levobupivacaine, 10ml of 0.25%, was administered epidurally in both the groups before incision of the surgery. 1 μg/kg of Dexmedetomidine was added to levobupivacaine10 ml of 0.25% in LD group while only Inj. Levobupivacaine was administered epidurally in L group at the time of skin closure of the surgical wound. Cardio-respiratory parameters, modified Ramsay sedation scores, VAS score for pain, time to first rescue analgesic and number of analgesic doses required in first 24 hours were recorded.
At the end of study, The data obtained was subjected to statistical computation with analysis of variance and chi-square test using statistical package for social science (SPSS) version 10.0 for windows and value of P < 0.05 was considered significant and P < 0.001 as highly significant.
Results: The demographic profile of patients was comparable in both the groups. 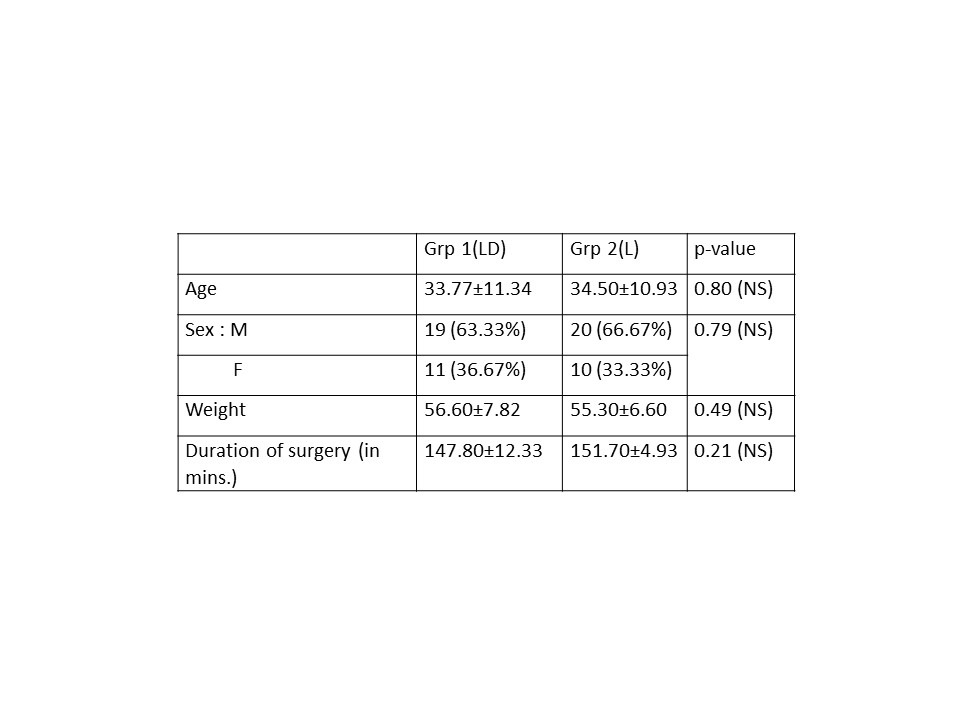 No. of doses of analgesics in first 24 hours were also less required in G1, 1.80±0.48 than G2 2.60±0.56 (p<0.01).
No. of doses of analgesics in first 24 hours were also less required in G1, 1.80±0.48 than G2 2.60±0.56 (p<0.01). 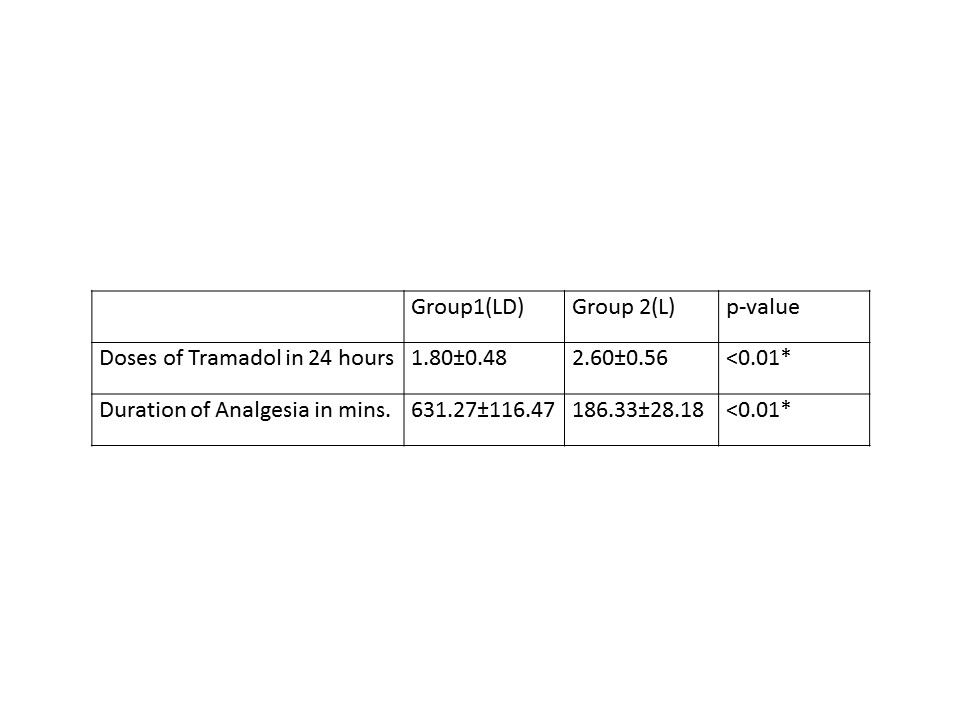 Postoperative analgesia (time to first rescue analgesia) was prolonged significantly in G1, 631.27±116.47 minutes than only G2, 186.33±28.18 minutes (p<0.01).
Postoperative analgesia (time to first rescue analgesia) was prolonged significantly in G1, 631.27±116.47 minutes than only G2, 186.33±28.18 minutes (p<0.01).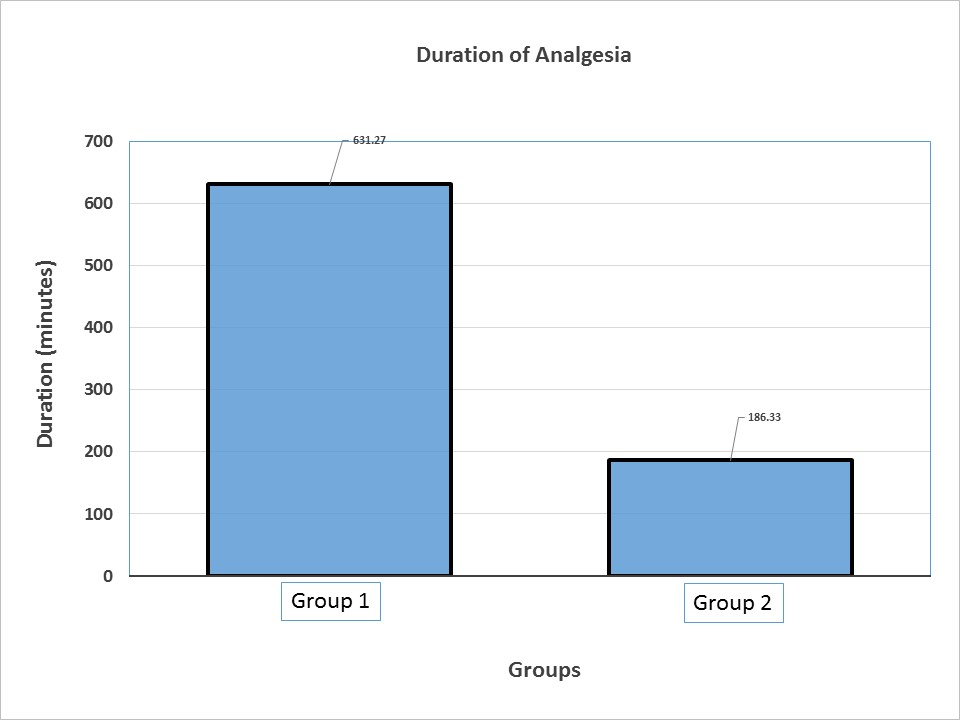 Postoperative sedation was observed in G1 group for initial period which was beneficial to the patients.
Postoperative sedation was observed in G1 group for initial period which was beneficial to the patients.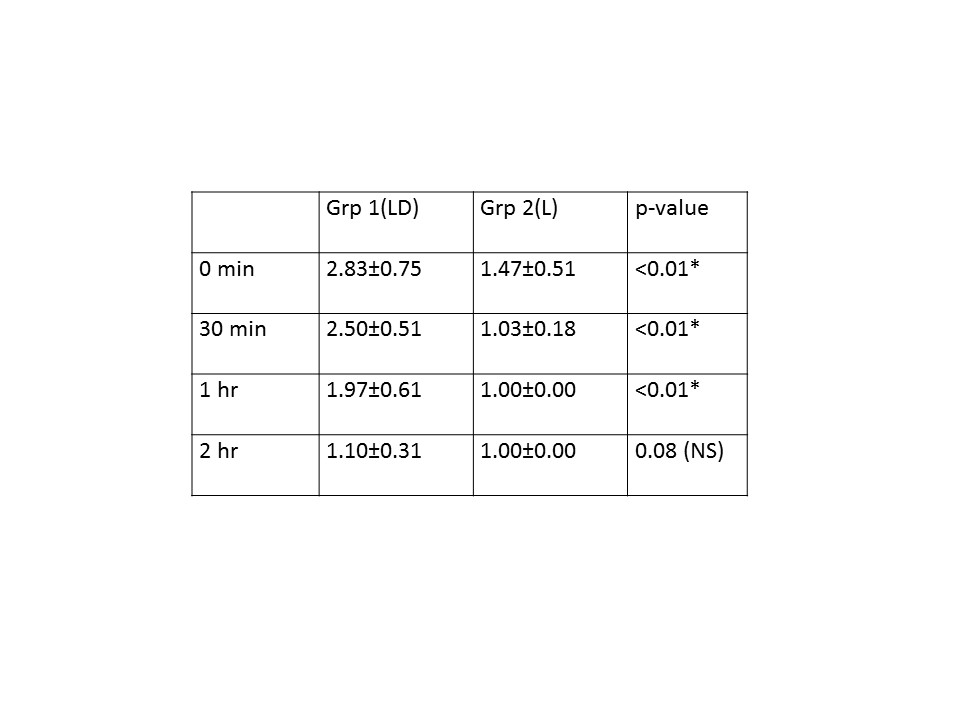 Incidence of side effects observed were minimum and non-significant in both the groups.
Incidence of side effects observed were minimum and non-significant in both the groups.
Conclusions: Dexmedetomidine seems to be a good epidural adjuvant to local analgesic as far as patient comfort, stable cardio-respiratory parameters and post-operative analgesia is concerned. It provides prolonged post-op analgesia, lower consumption of post-op analgesics, and much better sedation levels.
