Evaluation of Clonidine as an Adjuvant to Bupivacaine in Wound Infiltration for Providing Postoperative Analgesia After Laparoscopic Donor Nephrectomy
Bina Butala1, Geeta P. Parikh1, Rujal R. Patel1, Beena K. Parikh1, Kalpna S. Vora1, Manisha P Modi1, Veena R. Shah1.
1Department of Anesthesiology and Critical Care, Institute of Kidney Diseases and Research Centre & Institute of Transplantation Sciences, Ahmedabad, India
Introduction: Wound infiltration is a simple and effective means of providing postoperative analgesia. Clonidine as a peripheral analgesic, is an effective adjuvant to bupivacaine as a multimodal analgesia in patients with open cholecystectomy in post-operative period. We evaluated the 60 donors posted for laparoscopic nephrectomy for renal allograft recipients, for effectiveness of Clonidine as an adjuvant to bupivacaine in wound infiltration for postoperative analgesia in terms of quality and duration of postoperative analgesia in 30 donors as group-1 (G1) rather than bupivacaine used alone in 30 donors as group-2 (G2).
Materials and methods: This study is Institutional Review Board approved randomized prospective double blinded clinical study from January, 2015 to April, 2016 with written informed consent from 30 volunteer donors in each groups with American Society of Anesthesiologists I–II, planned for retroperitoneal laparoscopic donor nephrectomy. G1 received wound infiltration with 10 ml of 0.25% bupivacaine with 3 μg/kg clonidine and periportal infiltration with 10 ml of 0.25% bupivacaine with 3 μg/kg clonidine while G2 received wound infiltration with 10 ml of 0.25% bupivacaine and periportal infiltration with 10 ml of 0.25% bupivacaine.
A standard balanced general anesthesia technique was used in all the donors. Injectable Paracetamol 1 gm intravenous (IV) infusion given at the end of the surgery, and Diclofenac aqueous (75 mg.) IV used as rescue analgesic.
Visual analogue score (VAS) for pain, periodic effectiveness of analgesics before the first rescue analgesia, % of donors requiring rescue analgesic and total number of rescue analgesic doses in 24 h were compared between two groups.
Results: Clonidine group has lower pain score, longer duration of effective analgesia, lower % of patients requiring rescue analgesic and less number of doses of rescue analgesia in the first 24 hours (H).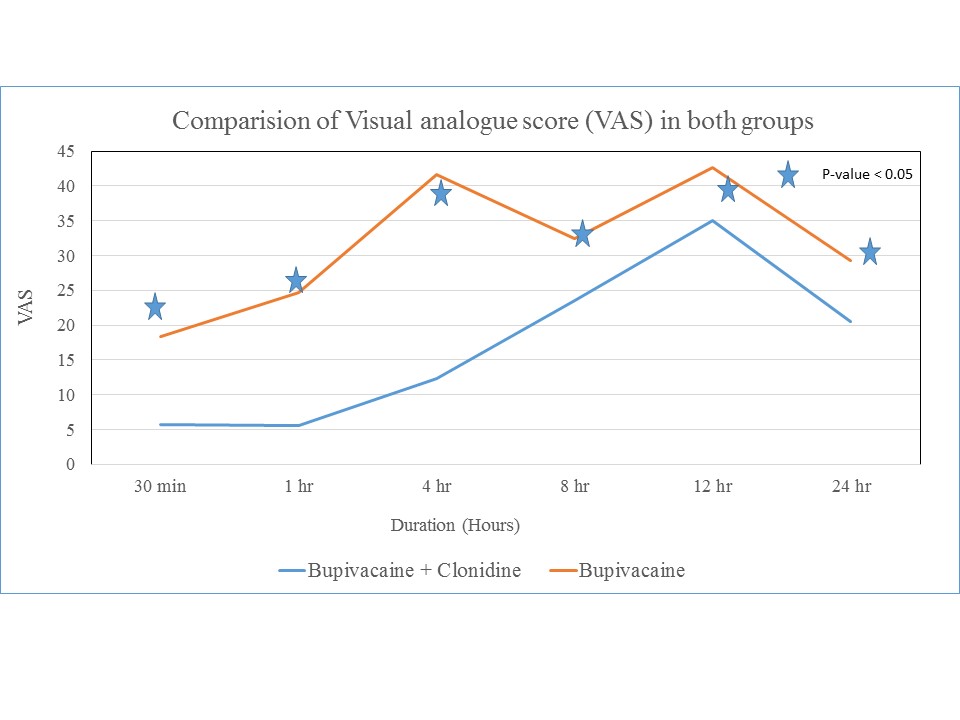 VAS was lower upto 12 H in G1and 4 H in G2. Effectiveness of analgesics lasted for 12-14 H in G1 and 4-5 H in G2. 70% and 100% of donors requiring rescue analgesic in G1 and G2 respectively.
VAS was lower upto 12 H in G1and 4 H in G2. Effectiveness of analgesics lasted for 12-14 H in G1 and 4-5 H in G2. 70% and 100% of donors requiring rescue analgesic in G1 and G2 respectively.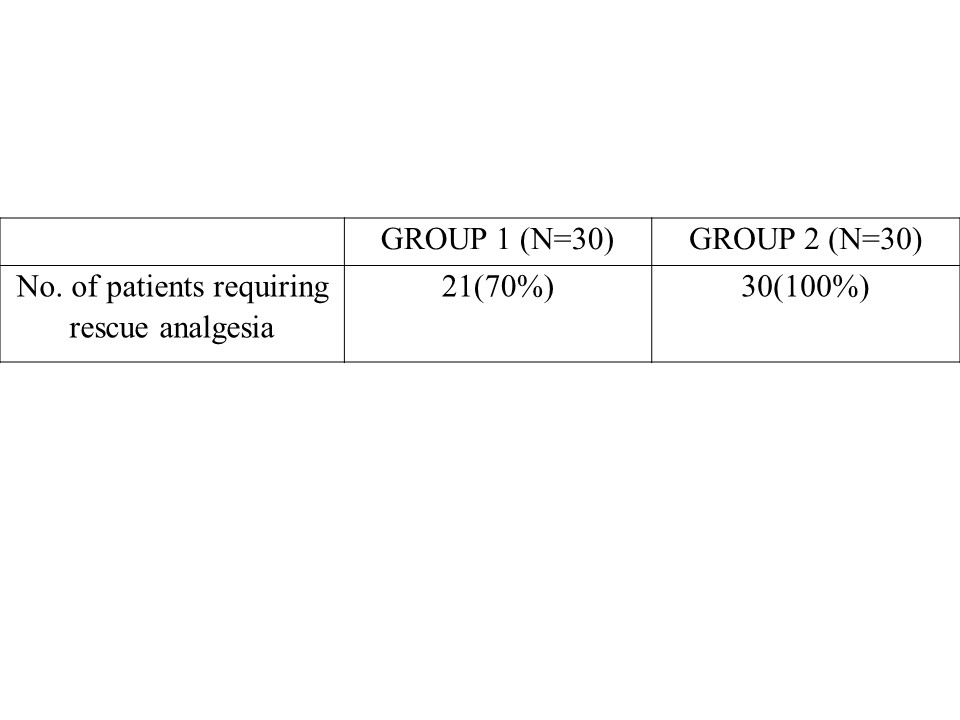 0.7±0.47 in G1 and 1.77±0.43 in G2, number of doses of rescue analgesia in the first 24 hours (H) required. Demographic and surgical parameters were comparable. Time for first request of analgesia
0.7±0.47 in G1 and 1.77±0.43 in G2, number of doses of rescue analgesia in the first 24 hours (H) required. Demographic and surgical parameters were comparable. Time for first request of analgesia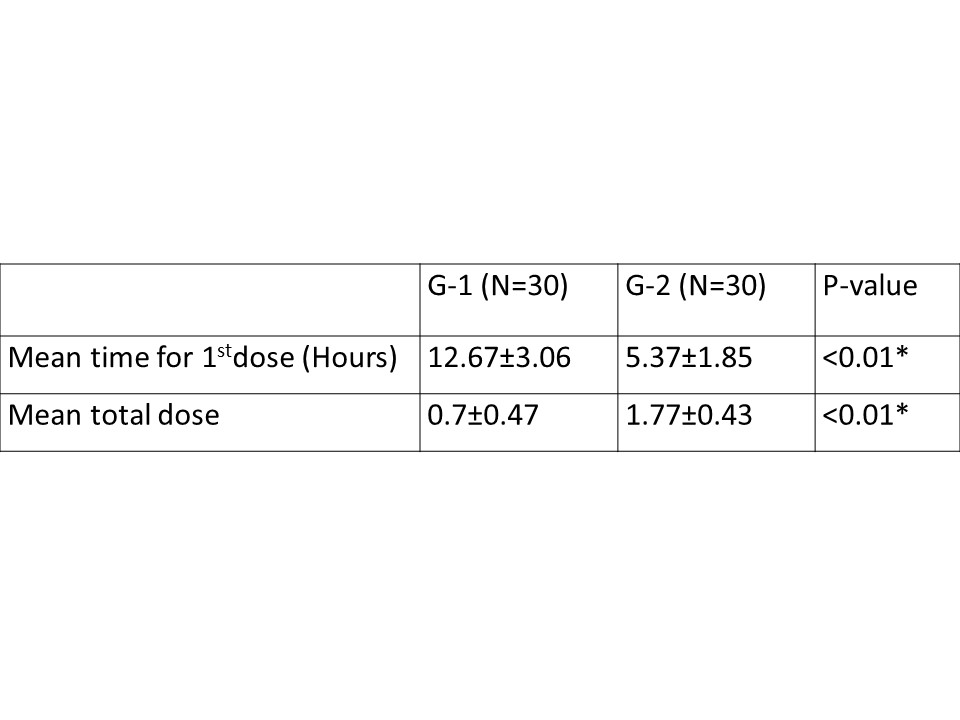 was prolonged in G1, 12.67 ± 3.06 H vs G2, 5.37 ± 1.85 H (P < 0.01), total Diclofenac consumption was significantly less (P < 0.01), and VAS was lower (P < 0.01) in G1 upto 12-14 h.
was prolonged in G1, 12.67 ± 3.06 H vs G2, 5.37 ± 1.85 H (P < 0.01), total Diclofenac consumption was significantly less (P < 0.01), and VAS was lower (P < 0.01) in G1 upto 12-14 h.
Conclusion: Clonidine 3 μg/kg is an effective adjuvant to Bupivacaine for wound infiltration in terms of quality and duration of postoperative analgesia following retroperitoneal laparoscopic donor nephrectomy as compared to Bupivacaine alone.
Discussion: Clonidine has vasoconstricting effect and augments the action of local anesthetics by interrupting the neural transmission of painful stimuli in A delta and C fibers.
