Obliterative Bronchiolitis Syndrome and Outcomes of Unplanned ICU Readmission Following Lung Transplantation
Cristopher Mazo Torre1, Teresa Pont1, Alberto Sandiumenge1, Maria Ballesteros2, Eloisa Lopez3, Ludy Rellan4, Juan Robles5, Jordi Rello1.
1Transplant Coordination Department, Vall d'Hebron University Hospital, Barcelona, Spain; 2Critical Care, Marqués de Valdecillas University Hospital, Santander, Spain; 3Critical Care, Hospital 12 de Octubre, Madrid, Spain; 4Critical Care, Hospital Universitario de A Coruña, A Coruña, Spain; 5Critical Care, Hospital Universitario Reina Sofia, Cordoba, Spain
Clinical Research/epidemiology In Pneumonia & Sepsis (CRIPS).
Introduction: Hospital re-admissions after lung transplant (LT) negatively affect quality of life, and costs. Reports on ICU readmission (ICU-r) have been limited to short series.
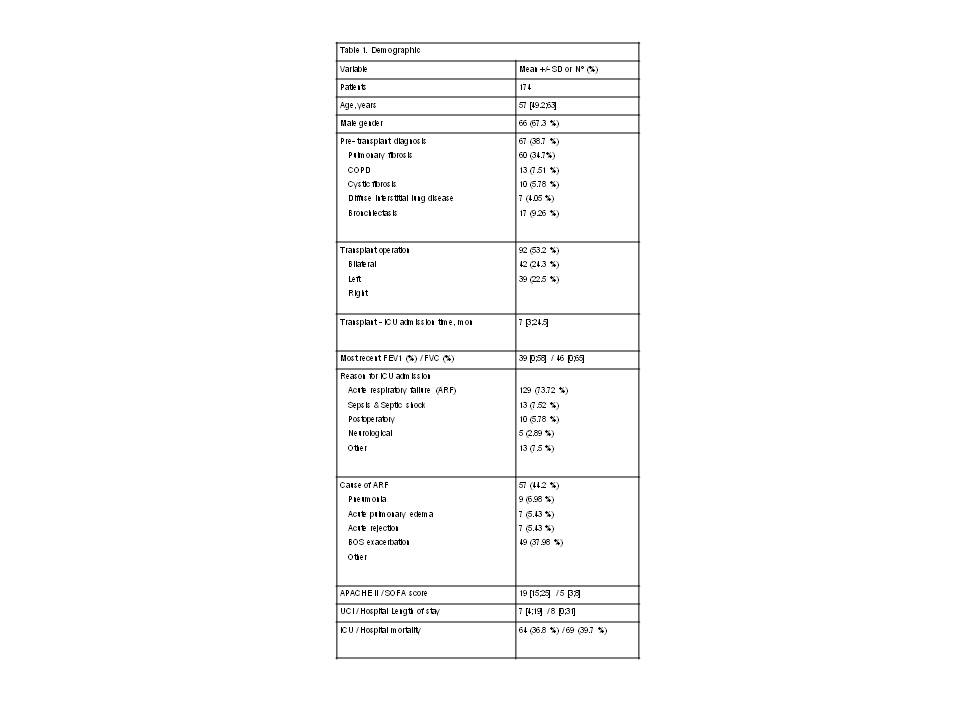
Methods:Prospective, multicenter, observational study including 174 consecutive LT adults requiring ICU-r (august 2012-16). We evaluated epidemiological features of this population and studied the outcomes.
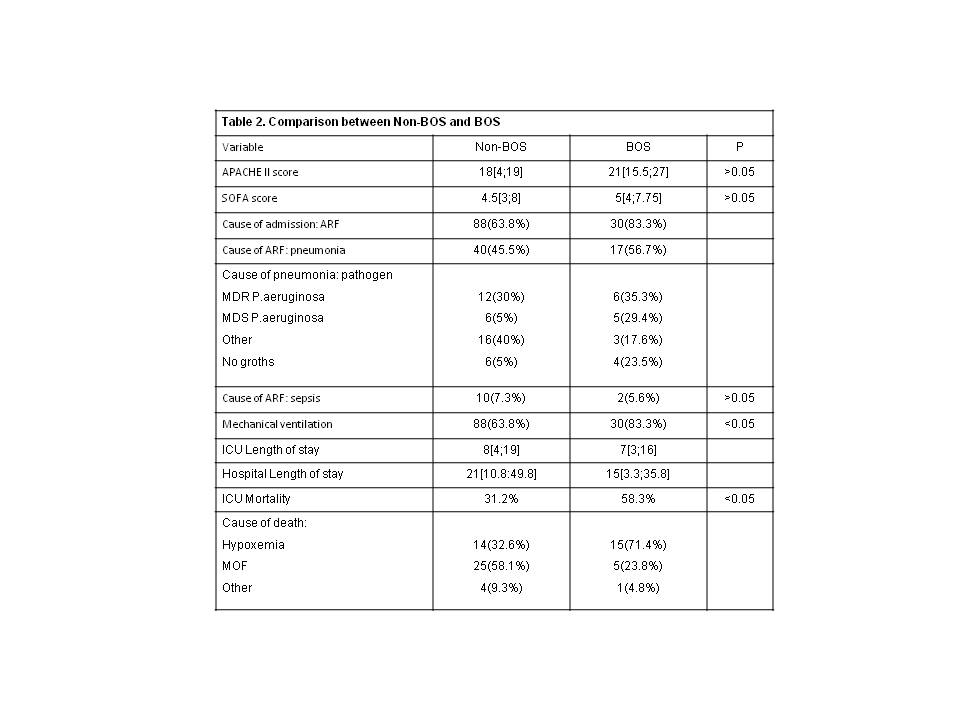
Results: Overall, 118 (68.2%) ICU-r were due to acute respiratory failure (ARF) and 78 (44.8%) had an infectious cause, with pneumonia the most prevalent (73%). Acute cellular and humoral rejection were identified in 12 (7%) and 2 (1%) respectively. Main lung diseases before transplant were pulmonary fibrosis (38.7%) and COPD (34.7%), 53.2% with bilateral transplant. (Table 1). When admitted by ARF, 90-day mortality was 44.2% (vs 26.4% when admitted by other causes, p<0.05). 90-day mortality for pneumonia was 49%. 36 patients (20.2%) ICU-r had obliterative bronchiolitis syndrome (BOS). Acute respiratory failure and pneumonia were more prevalent in BOS subgroup, BOS was significantly associated to higher requirement of mechanical ventilation, and ICU mortality. P. aeruginosa (most frequent MDR) was the pathogen isolated from both ICU-R with and without BOS. Hypoxemia was the main cause of death in patient with BOS, (Table 2)
Conclusions: Hypoxemia was the main cause of ICU readmission in LT, particularly within one year, whereas BOS showed association to prognosis.
FISS PI1401296 and CIBERES..
