Is the Lung Allocate Score Associated with the Decrease of the Primary Graft Dysfunction in Lung Transplantation?
Irene Bello1, Elisabeth Coll3, Alberto Sandiumenge2, Laura Romero1, Alberto Jauregui1, Javier Pérez1, Juan Manuel Ochoa1, Víctor Monforte5, Leire Sánchez1, Fernando Ascanio1, Pilar Montoya1, Judith Sacanell4, Anna González6, Teresa Pont2, Antonio Roman5, Maria Deu1.
1Thoracic Surgery, Vall d'Hebron Hospital, Barcelona, Spain; 2Transplant Coordination, Vall d'Hebron Hospital, Barcelona, Spain; 3Transplant National Organitation (ONT), Madrid, Spain; 4Intensive Unit Care, Vall d'Hebron Hospital, Barcelona, Spain; 5Pulmonology, Vall d'Hebron Hospital, Barcelona, Spain; 6Anestesiology, Vall d'Hebron Hospital, Barcelona, Spain
Background: On 2014 the system for allocation of lung recipients for transplant in HUVH changed from allocation based on waiting time to allocation based on the Lung Allocate Score (LAS score). We have analyzed the impact in primary graft dysfunction (PGD).
Methods: We retrospectively reviewed the cohort of 418 adult recipients of lung transplantation performed between 01/01/2010 and 02/08/2016 in our hospital. Patients were grouped by type of allocation: before LAS era(BLE) and after LAS era(ALE). Descriptive and comparative analysis of donors, recipients and procedures was performed between both groups to ensure comparability. Univariate and multivariate analysis were carried out to study factors influencing on PGD.
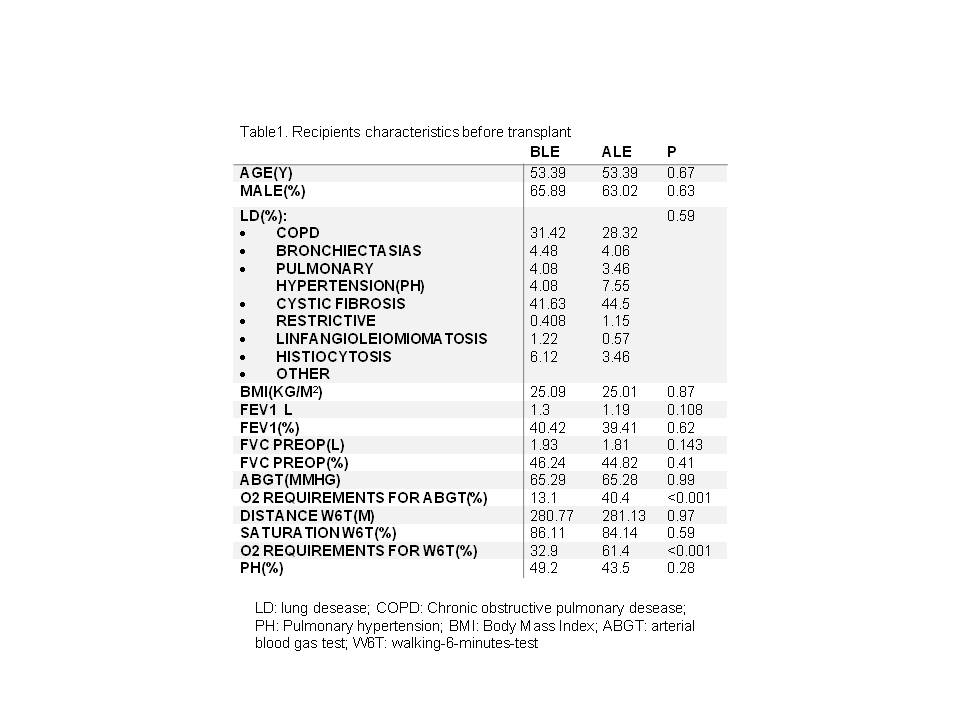
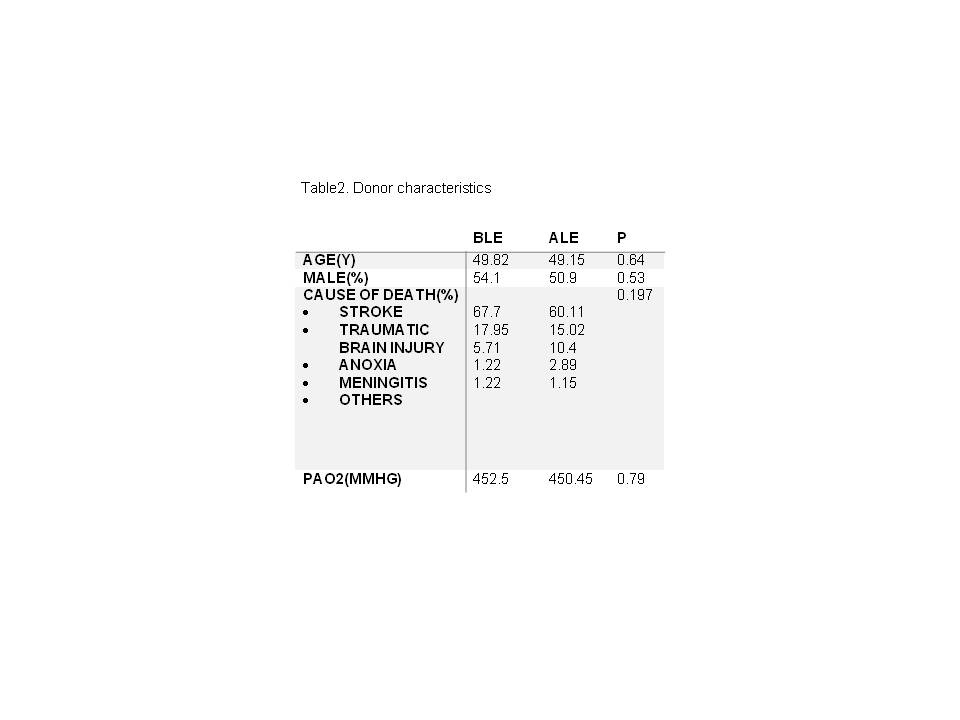
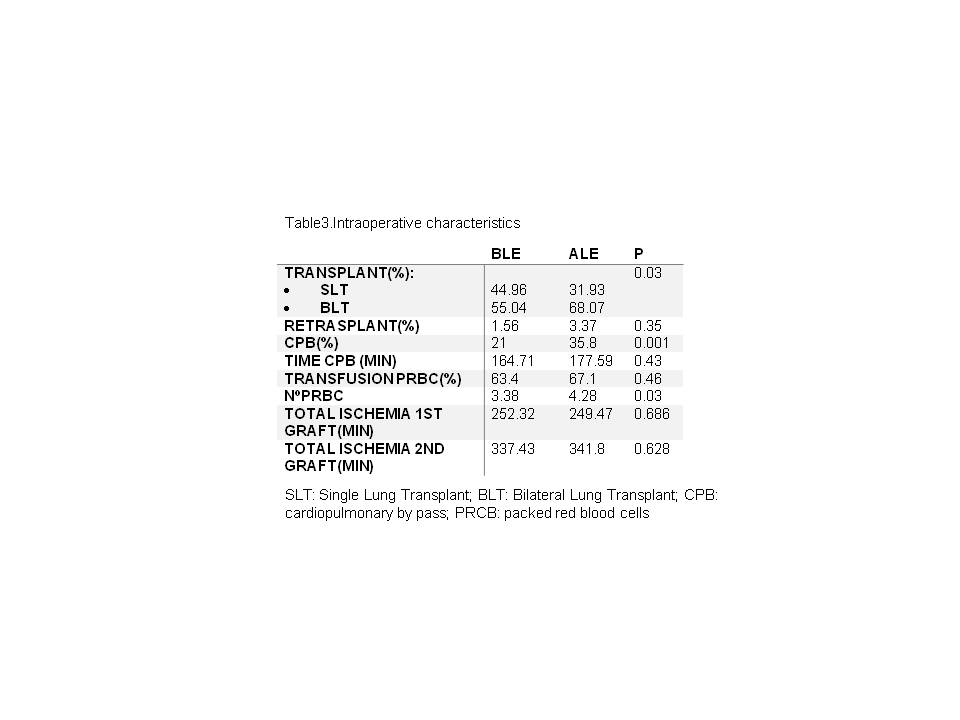
Results: There are not statistically significant differences in receptor’s age, gender, type of lung disease or donor characteristics (Table 1,2). The number of recipient who needed oxygen requirements for arterial blood gas test and walking-6-minutes-test before lung transplant was increased in ALE( 13.1% vs 40.4%, p=<0.001). During the procedure, cardiopulmonary bypass was needed more frequently in ALE (21% vs 35.8% p=<0.001) and recipients needed more packed red blood cells (3.38 vs 4.289, p=0.03) (Table 3). The incidence of PGD decreased in ALE(45.6% vs 32% p=0.007) (Table 4).After multivariante analysis, LAS was independently associated with a reduced risk for PGD( Table 5).
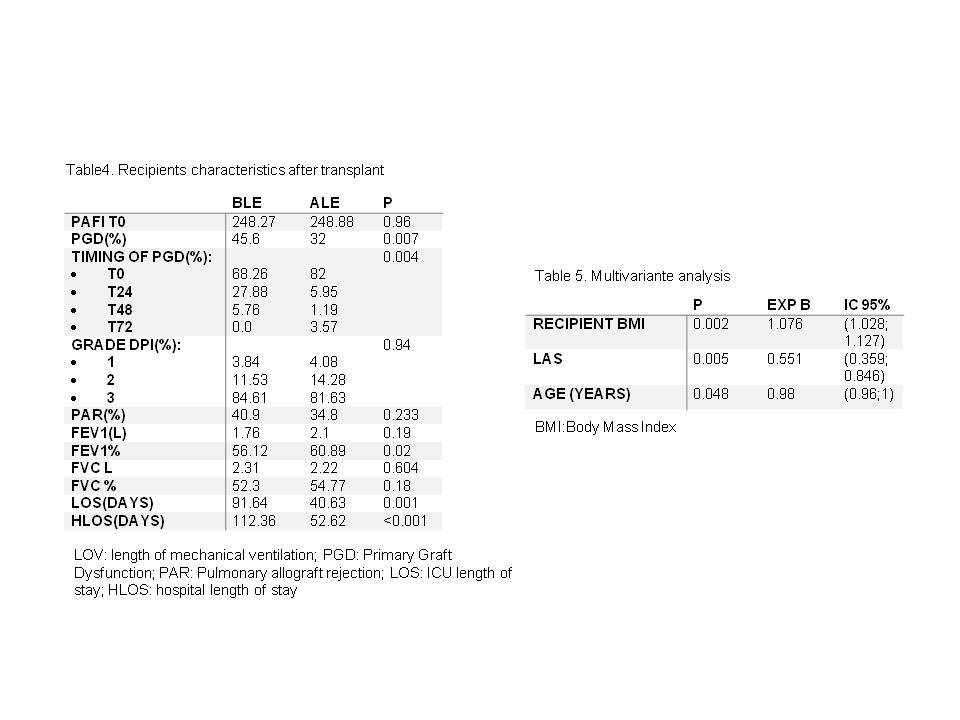
Conclusions: Allocating lungs for transplant based on urgency and benefit instead of waiting time is associated with reduced risk of PGD after lung transplantation.
