Impact of Allograft Ischemic Time on Short- and Long-term Survival in Lung Transplantation
Mohammed Fakhro1, Haider Ghaidan1, Lars Algotsson2, Hillevi Larsson3, Sandra Lindstedt1.
1Department of Cardiothoracic Surgery, Lund University, Lund, Sweden; 2Department of Thoracic Intensive Care and Anesthesia, Lund University, Lund, Sweden; 3Department of Pulmonary Medicine, Lund University, Lund, Sweden
Purpose: The influence of allograft ischemic time (IT) on short- and long-term mortality remains under debate in lung transplantation (LTx). Due to a scarcity in donors it might be possible to improve the outcome in LTx by investigating associations and characteristics in IT among different recipients. This report studied the effect of IT among different patient groups in both short- and long-term mortality in LTx .
Methods: Between January 1990 to June 2016; 307 patients underwent LTx at Lund university hospital, Sweden. In addition, 18 patients required re-transplantation (Re-LTx). IT was defined as the mean elapsed time between cross-clamp of the aorta at organ harvest until reperfusion during transplantation. The end-point used was death or Re-LTx assessed by Cox regression and Kaplan-Meier survival.
Results: Survival curves for mean IT (min) between subgroups ≤120, 121-240, 241-360 and 361+ are shown in image 1 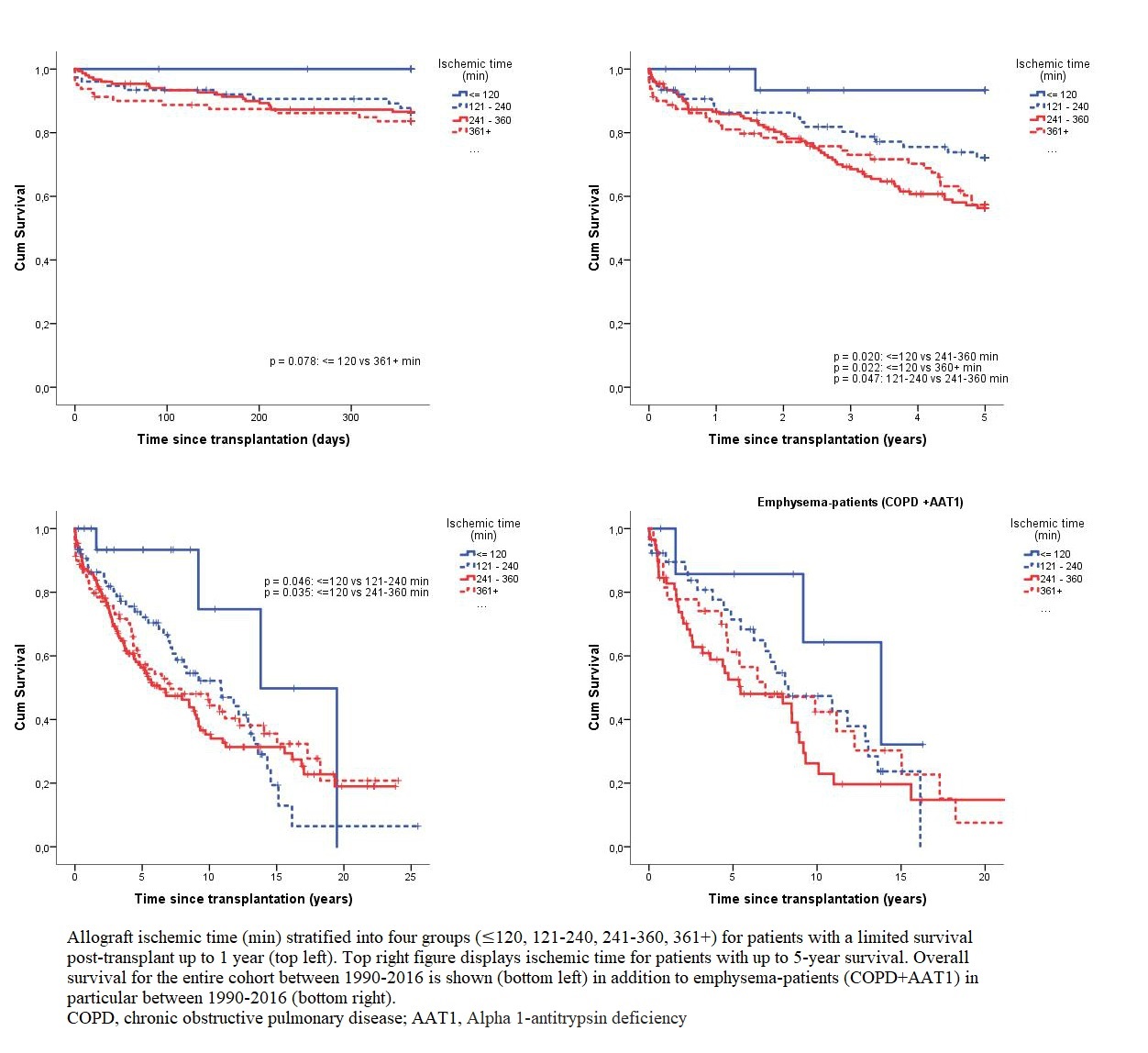 . IT in patients with a limited survival up to 1- and 5-year had a hazard ratio (HR) of 1.002 and 1.001 respectively (p<0.05) while overall long-term survival had a HR of 1.000 and a HR of 1.001 in emphysema-patients in particular (p>0.05). Significance was kept when adjusted for age, Tx-type and Tx-year. No assocation was found in interaction between IT and recipient BMI or age (p>0.05).
. IT in patients with a limited survival up to 1- and 5-year had a hazard ratio (HR) of 1.002 and 1.001 respectively (p<0.05) while overall long-term survival had a HR of 1.000 and a HR of 1.001 in emphysema-patients in particular (p>0.05). Significance was kept when adjusted for age, Tx-type and Tx-year. No assocation was found in interaction between IT and recipient BMI or age (p>0.05).
Conclusion: In LTx, every 2-hour increase of IT is equivalent to an increased mortality of up to 24% within 5-years. However, an increased IT in interaction with recipient age/BMI did not seem to further affect post-Tx survival. LTx with an IT of ≤120 min had a superior survival in both 1- and 5-years in comparison to an IT of up to 360 min. In long-term survival no difference was shown in recipients ranging between 120-360 min. With emphysema-patients having the lowest presented survival rates, no survival benefit was shown among different IT groups. By incorporating these findings into a more customized organ allocation program it is possible to maximize the number of LTx in an already scarce donor pool and improve the outcome in LTx.
