Ultrastructural Changes in Lung Allografts: Endothelial Changes Correlate with Donor Specific Antibody and Antibody-Mediated Rejection
Mariam Alexander1, Andrew Bentall3, Patrice C Abell Aleff2, John P SCott4, Anja C Roden1.
1Department of Laboratory Medicine and Pathology, Mayo Clinic, Rochester, MN, United States; 2Department of Biochemistry and Molecular Biology, Mayo Clinic, Rochester, MN, United States; 3Division of Nephrology and Hypertension, Mayo Clinic, Rochester, MN, United States; 4Division of Pulmonary and Critical Care Medicine, Mayo Clinic, Rochester, MN, United States
Introduction: Antibody mediated rejection (AMR) is a well-recognised cause of allograft injury; however only recently there is a growing recognition in lung transplantation (LTx). Allograft dysfunction can be multifactorial and challenges with C4d stain interpretation and the lack of specificity of histological criteria account for some of the difficulties in diagnosing pulmonary AMR. Donor Specific Antibodies (DSA) target the endothelium. In fact, in renal transplantation, endothelial activation markers and early ultrastructural changes of the endothelium correlate with AMR. The aim of this study was to identify ultrastructural changes in the endothelium of lung allografts in the presence of DSA, with the intent of determining if prospective use of electron microscopy might be helpful in establishing a diagnosis of AMR in LTx recipients.
Materials & Methods: The LTx database was queried for cases of pulmonary AMR between 07/2009 & 09/2015. The ISHLT guidelines were used to categorise these cases into definite, probable & possible AMR. Retrospective ultrastructural studies were performed on all these biopsies- either fresh or paraffin embedded. Cases of acute cellular rejection (4) and normal lung (3) were evaluated as controls. The findings on ultrastructural examination were correlated with the presence of DSA & diagnosis of AMR using the Pearson’s chi-square test of statistical significance.
Results & Discussion: Eleven patients (male, 54.5%) were included in this study. 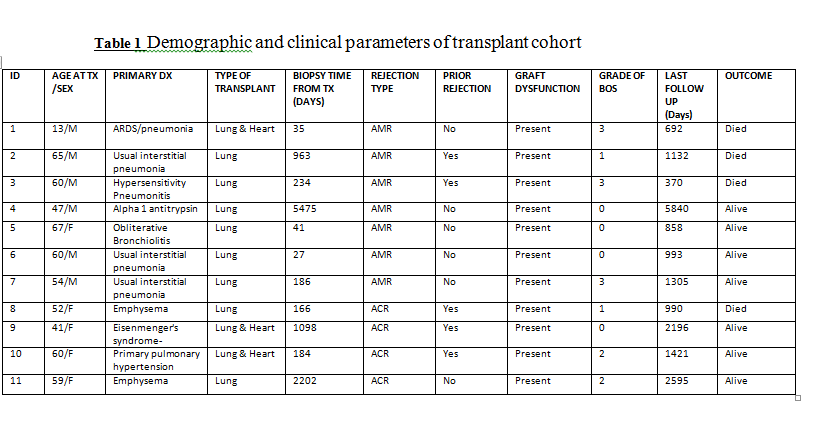 Mean age was 53yrs. Three cases were combined lung & heart Tx. We identified 7 cases of AMR (1 definite, 1 probable & 5 possible). The median time from LTx to biopsy (bx) was 210 days, with median follow up of 1063 days. Bronchiolitis Obliterans Syndrome was diagnosed in 5 patients. Ultrastructural studies were performed on 10 AMR bxs (pt 6:2 bxs; pt 7:3 bxs; all other pts: 1bx each), 4 ACR bxs & 4 controls. The results are shown.
Mean age was 53yrs. Three cases were combined lung & heart Tx. We identified 7 cases of AMR (1 definite, 1 probable & 5 possible). The median time from LTx to biopsy (bx) was 210 days, with median follow up of 1063 days. Bronchiolitis Obliterans Syndrome was diagnosed in 5 patients. Ultrastructural studies were performed on 10 AMR bxs (pt 6:2 bxs; pt 7:3 bxs; all other pts: 1bx each), 4 ACR bxs & 4 controls. The results are shown. 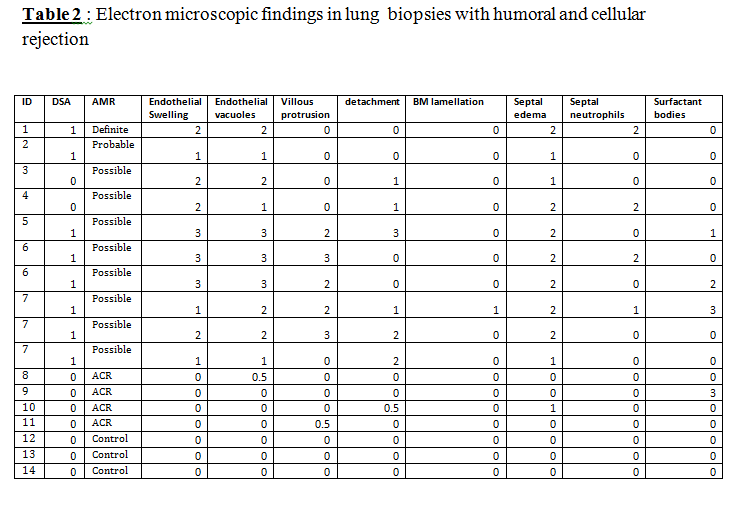 The presence of DSA as well as the ISHLT diagnosis of AMR significantly correlated with endothelial swelling, cytoplasmic vacuolisation & septal edema (p<0.01; each). Septal infiltration by neutrophils was only identified in AMR cases, although it did not achieve statistical significance. Importantly, these differences were still significant when using resin or paraffin based samples for EM, allowing larger retrospective studies to be performed; although endothelial swelling & vacuolisation occurred in non-DSA paraffin samples with EM.
The presence of DSA as well as the ISHLT diagnosis of AMR significantly correlated with endothelial swelling, cytoplasmic vacuolisation & septal edema (p<0.01; each). Septal infiltration by neutrophils was only identified in AMR cases, although it did not achieve statistical significance. Importantly, these differences were still significant when using resin or paraffin based samples for EM, allowing larger retrospective studies to be performed; although endothelial swelling & vacuolisation occurred in non-DSA paraffin samples with EM.
Conclusion: Donor specific anti-HLA antibodies are associated with endothelial injury of the allograft. Ultrastructural findings such as endothelial swelling & vacuolization help in diagnosing antibody mediated allograft injury. Although paraffin embedded biopsy material can be used for this purpose, it is not without limitations and larger prospective studies are needed to validate these findings. The effect of DSA on the endothelial pathways will be important in all solid organ transplantation.
