Liver Transplantation in Children with Hepatoblastoma: A Single-Center 30 Year Experience Examining Prognostic Factors for Survival and Recurrence
Douglas Farmer1, Robert S Venick2, Samer Ebaid1, Noah Federman3, Vatche G Agopian1, Joseph DiNorcia1, Fady M Kaldas1, Jorge Vargas2, Ronald W Busuttil1, Suzanne V McDiarmid2.
1Surgery, David Geffen School of Medicine at UCLA, Los Angeles, CA, United States; 2Pediatrics, Mattel UCLA Children's Hospital, Los Angeles, CA, United States; 3Hematology-Oncology, Mattel UCLA Children's Hospital, Los Angeles, CA, United States
Background: Liver transplantation (LTx) is a well-established treatment for unresectable hepatoblastoma (HBA) in children. However, assessment of outcomes is limited as there are few published experiences. This study aimed to describe in detail and identify risk factors for survival for HBA following LTx at one of the largest single-center experiences.
Methods: All children ≤ 18 y/o who underwent LTx for HBA between 3/1984 to 10/2017 were included in analysis. Median follow up was 61 mo. Over 25 demographic, laboratory, operative, donor and recipient variables were analyzed using Log-Rank and Cox-Proportional Hazards model.
Results: 45 HBA (4.4%) out of the 1021 isolated LTx were included in analysis. The majority were male (58%). The median age at diagnosis was 20 mo. Median AFP was 285,000 ng/mL. PRETEXT stages were II (4), III (21), IV (20). Extrahepatic disease was present in 4 and vascular invasion in 14 at presentation. Treatments prior to LTx included: chemotherapy (43), TACE (7), and surgical resection (15)
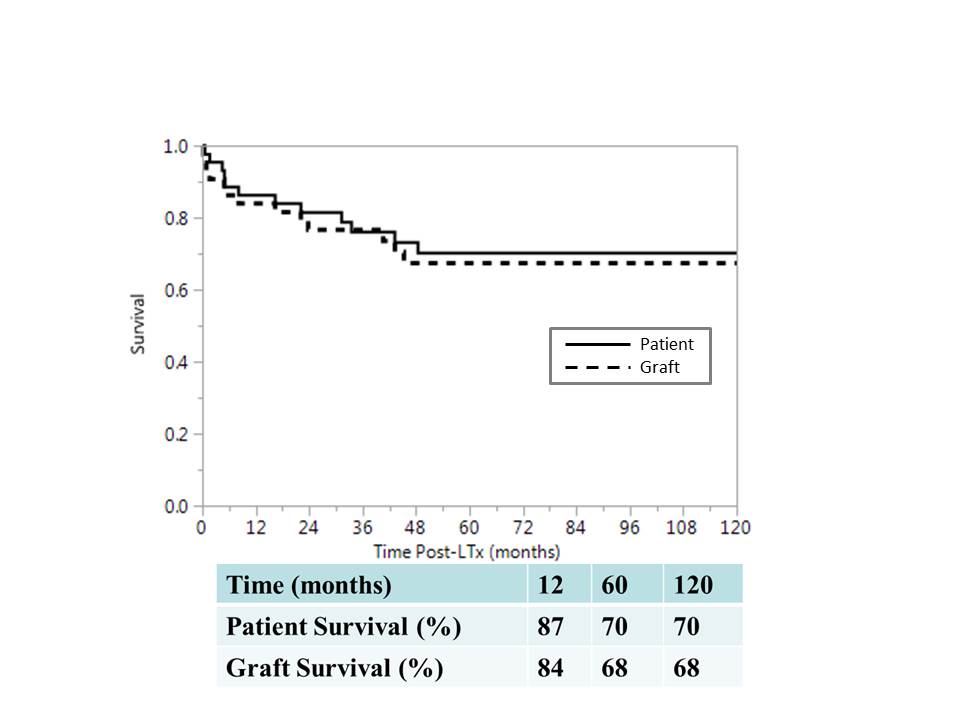
The median age at LTx was 31 mo. Whole grafts were used in 84%. Explant pathology revealed LN+ (3), vascular invasion (18), lymphatic invasion (6). Post LTx chemotherapy was administered in 84%. Complications included HBA recurrence (20%) and HAT (20%). Patient and graft survival is shown in FIGURE 1.
Covariates found to be insignificant predictors of patient survival: gender (p=0.61), ethnicity (p=0.29), AFP at diagnosis <1 million (p=0.38), histology- epithelial vs. mixed (p=0.60), number of nodules- unifocal vs. multifocal (p=0.41), microscopic intrahepatic lymphatic invasion at time of LTx (p=0.39), local lymph nodes + at time of LTx (p=0.79)
Covariates found to approach significance as predictors of patient survival: PRETEXT Stage (p=0.12), segmental graft (p=0.06),
Covariates found to be significant predictors of patient survival: lung mets at diagnosis (0 <0.0001), macrovascular involvement (p=0.03), microscopic intrahepatic microvascular invasion at time of LTx (p=0.0005), resection prior to LTx (p=0.04).
Conclusions: This study represents one of the largest single-center experiences with LTx in children with HBA. Excellent survival can be obtained in this high-risk population. The HAT rate is 3x higher than in our overall pediatric LTx experience and may relate to a thrombophilic condition associated with malignancy and chemotherapy. Several important variables were identified and confirmed as prognosticators of poor outcome. The strongest predictors indicate that resection should be avoided in cases where recurrence is likely, whole grafts should be preferentially applied in select cases, and careful consideration must be given to patients with obvious vascular invasion and metastatic disease at the time of presentation.