Inflammatory Frailty Index and Mortality after Kidney Transplantation
Christine Haugen1, Hao Ying 1, Mara McAdams-DeMarco1,2, Dorry L Segev 1,2.
1Surgery , Johns Hopkins Hospital , Baltimore , MD, United States; 2Epidemiology , Johns Hopkins Bloomberg School of Public Health , Baltimore , MD, United States
Frailty is a clinical phenotype of decreased physiologic reserve to stressors and is associated with a pro-inflammatory state. Fried frailty (measured by 5 components: slowed walk speed, unintentional weight loss, decreased grip strength, low physical activity, and exhaustion) was developed and validated in community dwelling older adults and is associated with poor outcomes after kidney transplant (KT) including mortality, longer length of stay after KT, early hospital readmission, and delayed graft function. However, Fried frailty does not directly capture inflammatory biomarkers like interleukin 6 (IL6) and tumor necrosis factor alpha (TNFalpha) that are associated with increased post-KT mortality. Therefore, we sought to identify a novel frailty index that combines inflammatory biomarkers and measured physical components.
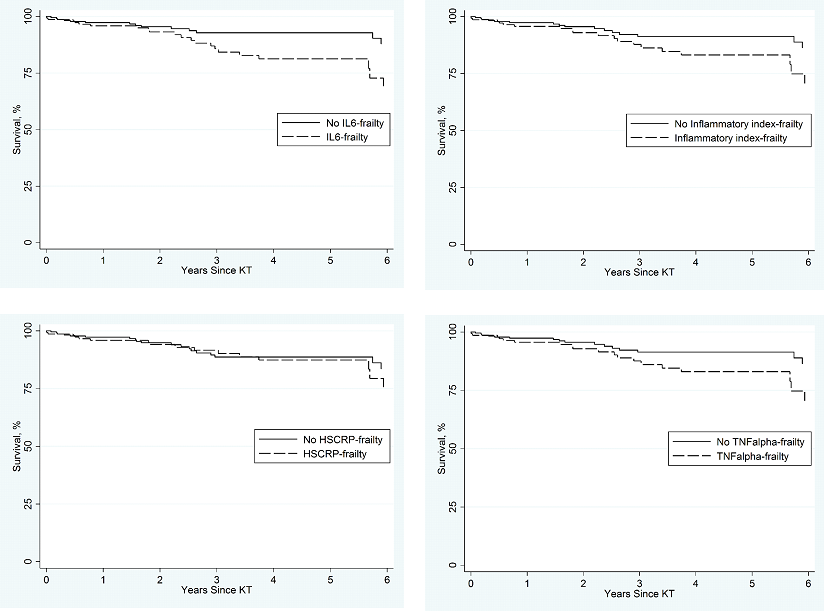
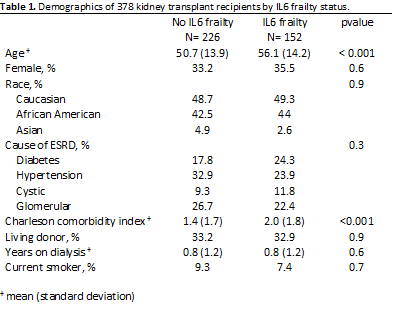
Methods: We identified 378 KT recipients at Johns Hopkins Hospital from 2009-2013 who consented to enrollment in a prospective cohort. Fried frailty and inflammatory markers (IL6, TNFalpha, highly sensitive C reactive protein [(HSCRP]) were collected at the time of admission for KT. We evaluated novel inflammatory-frailty indices combining Fried frailty phenotype (comprised of 5 components) plus the addition of individual inflammatory biomarkers (highest tertile of IL6, TNFalpha, HSCRP, or inflammatory index, separately) as a 6th component. Therefore, scores for each novel inflammatory frailty index were 0-6 points, and the presence of ≥3 components was considered frail. We used Kaplan-Meier methods and Cox proportional hazards model to assess mortality risk after KT by inflammatory frailty index. We adjusted Cox models for recipient age, sex, race, Charlson comorbidity index, and donor type.
Results: Five-year survival for patients with and without each novel inflammatory frailty index for frail vs nonfrail was: 81% vs 93% (IL6-frailty), 87% vs 89% (HSCRP-frailty), 83% vs 91% (TNFalpha-frailty), and 83% vs 91% (Inflammatory index-frailty). After adjustment, mortality was 2.04-fold higher for IL6-frail recipients compared to non-IL6-frail (95%CI:1.02-4.10, p=0.05); there were no associations between the mortality and the other inflammatory-frailty indices (HSCRP-frail:1.01,95%CI:0.51-0.98,p=0.9; TNFalpha-frail:1.94,95%CI:0.98-3.83,p=0.06; or inflammatory index-frail:1.66,95%CI:0.84-3.30,p=0.14) recipients. After adjustment, mortality was similar between nonfrail and frail KT recipients measured with Fried frailty (1.63,95%CI:0.75-3.51, p=0.2) and the highest tertile of IL-6 (1.37,95%CI:0.68-2.73, p=0.4).
Conclusions: IL-6 frailty is a unique frailty phenotype, combining biomarkers and physical components that improves upon the Fried frailty phenotype and is more strongly associated with post-KT mortality. Measurement of biomarkers at KT evaluation and transplantation can guide risk assessment and patient counseling.
National Institutes of Health .
