Impact of Donor-Specific Anti-HLA Antibodies on Chronic-Active Antibody-Mediated Rejection Histological Phenotype and Outcome is Modulated by Non-Adherent behavior of Kidney Graft Recipients
Jorge Malheiro1, Sofia Santos1, Sandra Tafulo2, Leonídio Dias1, La Salete Martins1, António Castro-Henriques1.
1Nephrology & Kidney Transplantation Unit, Centro Hospitalar do Porto, Porto, Portugal; 2Histocompatibility Lab, IPST, Porto, Portugal
Chronic-active antibody-mediated rejection (CAABMR) is a histo-clinical entity, associated with poor kidney graft survival, and without effective therapeutic interventions. Detailing correlations between clinical, immunological and histological characteristics with CAABMR prognosis would be important in order to better understand this entity.
Forty-one cases of CAABMR were detected in clinically-driven kidney graft biopsies. All cases had a cg score ≥ 1, 39 (95%) had microvascular inflammation score (g+ptc) ≥2, 24 (59%) had DSA at time of graft biopsy and 9 (22%) had a C4d score ≥1. We sought to investigate DSA and adherence status impact on histological phenotype and prognosis in these cases.
Non-adherence was defined as patient admission of medication non-adherence documented by clinic staff and/or drug levels below the detectable limit. Additionally, we calculated calcineurin inhibitor coefficient of variation (CV).
| Total (n=41) | Cyclosporine (n=15) | Tacrolimus (n=26) | |||||||
| Adherent | Non-adherent | P | Adherent | Non-adherent | P | Adherent | Non-adherent | P | |
| CV (%)(IQR) | 15.0 (9.9-21.3) | 35.1 (27.5-41.1) | <0.001 | 12.3 (8.2-18.5) | 32.6 (28.0-46.7) | 0.001 | 17.0 (12.9-21.9) | 35.1 (25.6-61.3) | <0.001 |
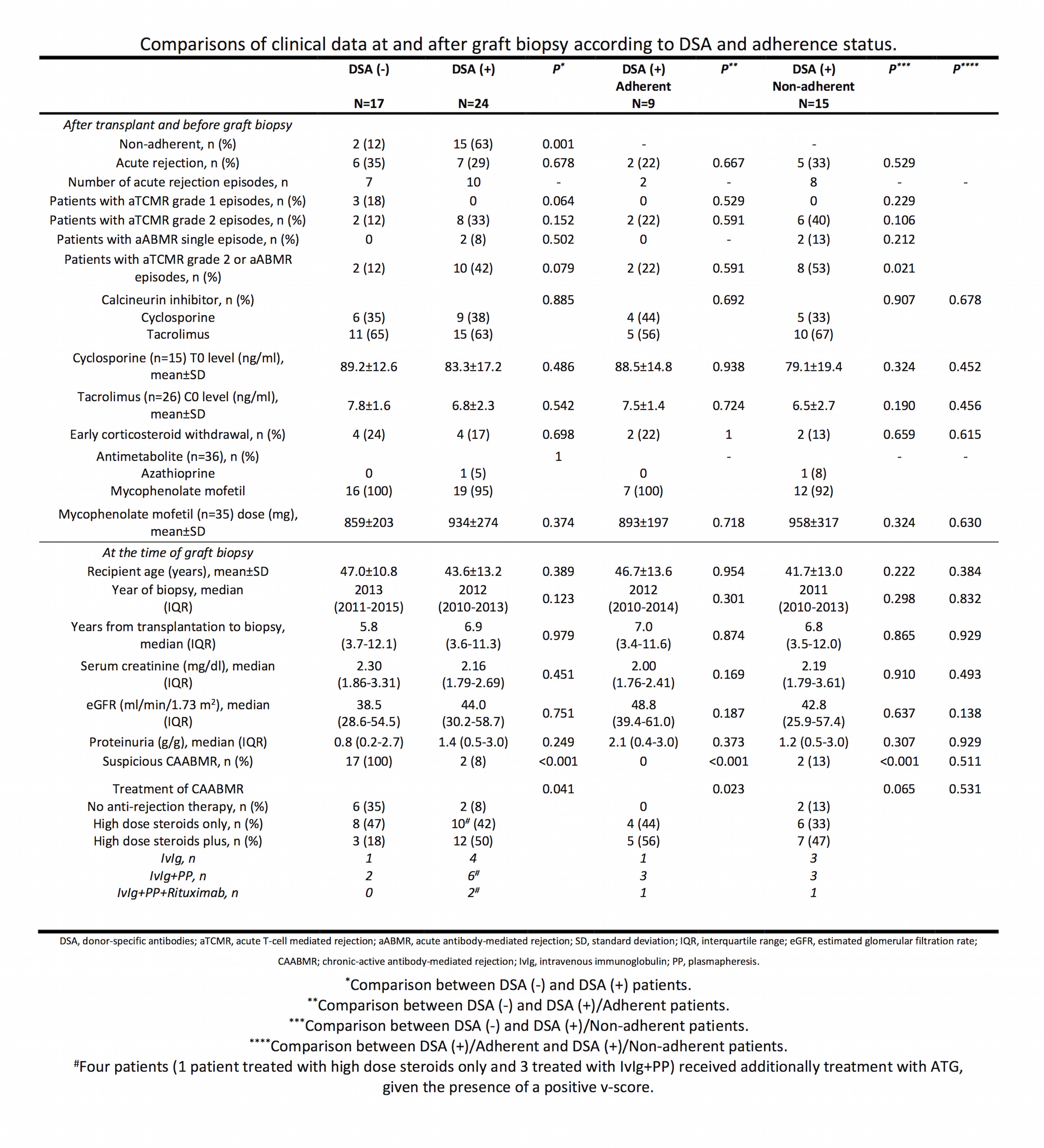 No difference in DSA characteristics (number, HLA class, strength) was detected between adherent and non-adhenrent patients, in the DSA (+) group.
No difference in DSA characteristics (number, HLA class, strength) was detected between adherent and non-adhenrent patients, in the DSA (+) group.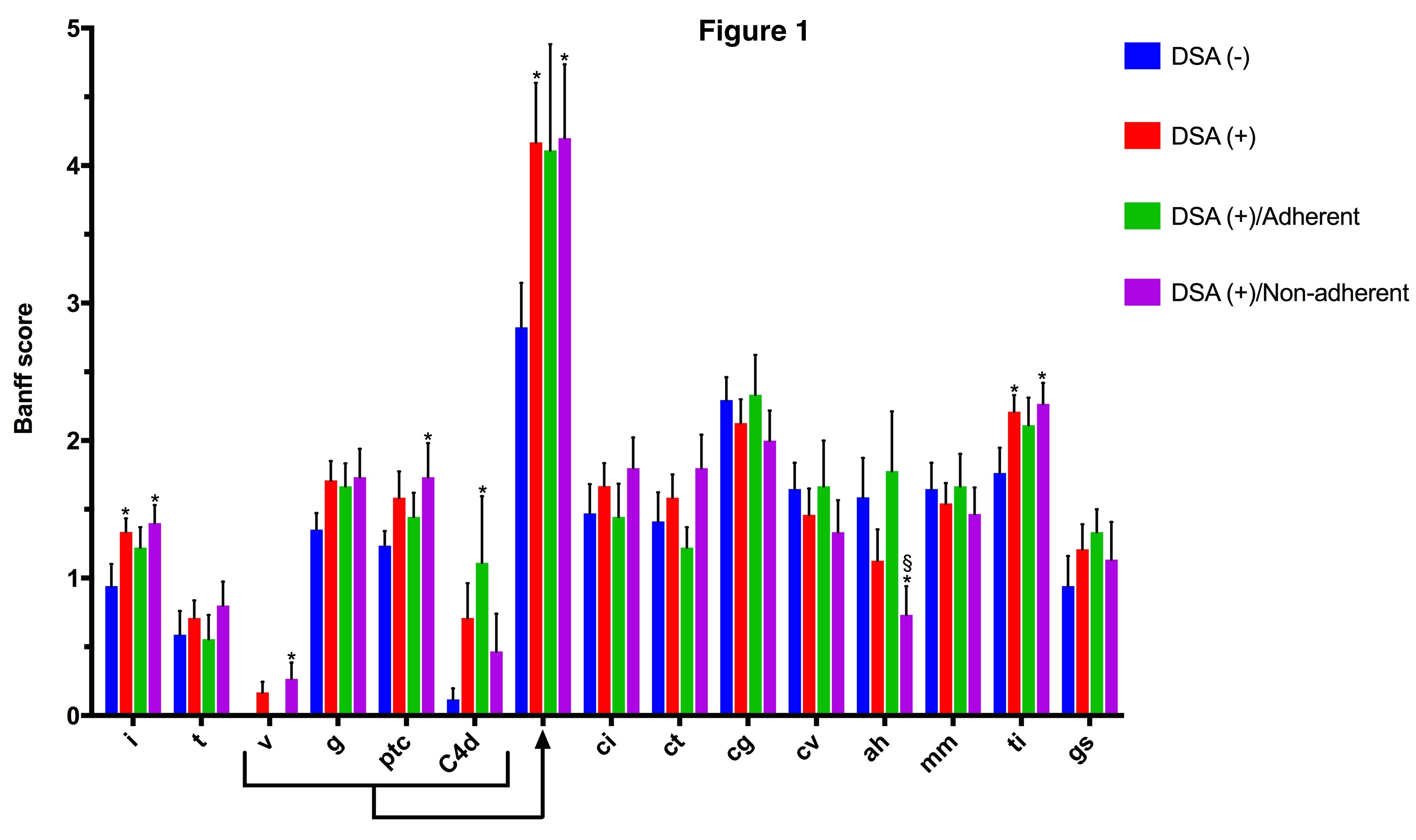 Figure 1. Comparison of histopathological scores according to DSA and adherence status. Bars indicate mean and T bars indicate standard error of mean. *P<0.050 between DSA (-) group versus any other of the 3 groups. §P<0.050 between DSA (+)/Adherent versus DSA (+)/Non-Adherent groups. Also shown is the composite acute humoral score (g+ptc+v+C4d).
Figure 1. Comparison of histopathological scores according to DSA and adherence status. Bars indicate mean and T bars indicate standard error of mean. *P<0.050 between DSA (-) group versus any other of the 3 groups. §P<0.050 between DSA (+)/Adherent versus DSA (+)/Non-Adherent groups. Also shown is the composite acute humoral score (g+ptc+v+C4d).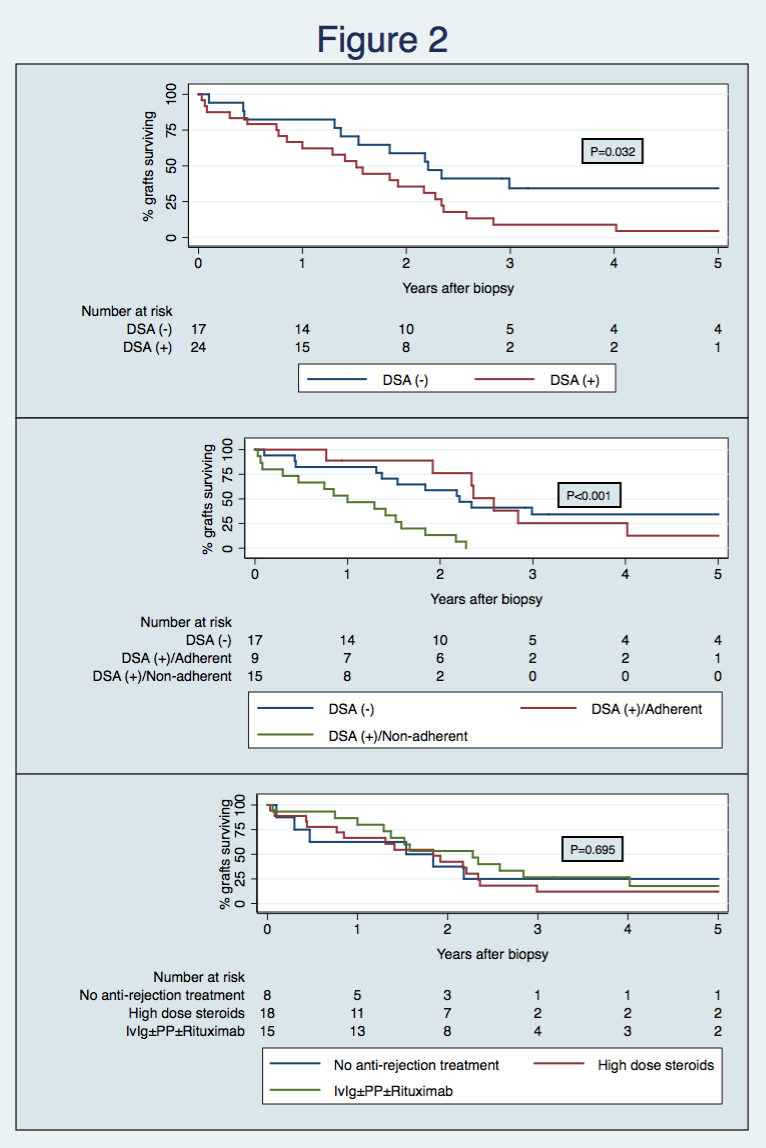 Figure 2. Top. Kaplan-Meier graft survival curves according to DSA status [median survival at 5-years post-transplant, DSA (-) 34.3% and DSA (+) 4.4%]. Middle. Kaplan-Meier graft survival curves according to DSA and adherence status [survival at 5-years post-transplant, DSA (-) 34.3%, DSA (+)/Adherent 12.7% and DSA (+)/Non-adherent 0%]. Bottom. Kaplan-Meier graft survival curves according to treatment strategy [survival at 5-years post-transplant, no anti-rejection treatment 25.0%, high dose steroids 12.1% and IvIg±PP±Rituximab 17.8%].
Figure 2. Top. Kaplan-Meier graft survival curves according to DSA status [median survival at 5-years post-transplant, DSA (-) 34.3% and DSA (+) 4.4%]. Middle. Kaplan-Meier graft survival curves according to DSA and adherence status [survival at 5-years post-transplant, DSA (-) 34.3%, DSA (+)/Adherent 12.7% and DSA (+)/Non-adherent 0%]. Bottom. Kaplan-Meier graft survival curves according to treatment strategy [survival at 5-years post-transplant, no anti-rejection treatment 25.0%, high dose steroids 12.1% and IvIg±PP±Rituximab 17.8%].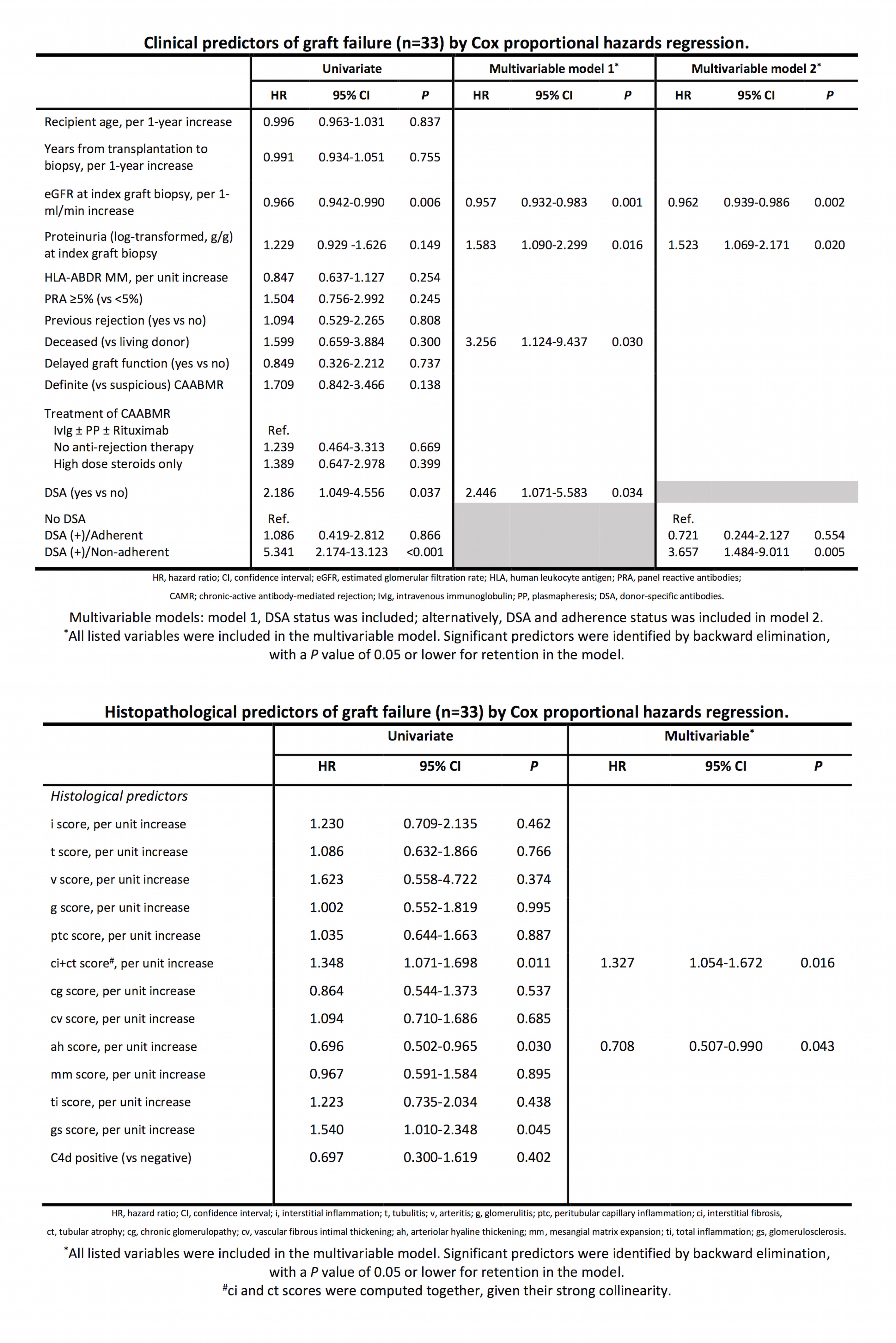 Concomitant presence of DSA in CAABMR cases is associated with poorer kidney graft survival, particularly if non-adherence is also documented. Histological phenotype in DSA (+)/non-adherent cases show a simultaneous cellular and antibody-mediated pattern of injury, with higher interstitial of inflammation and acute humoral scores. Additionally, ah score was significantly reduced in these patients, showing arteriolar under-hyalinosis correlation with under-immunosuppression and, importantly, correlated inversely with graft failure. No anti-rejection treatment strategy correlated with an improved graft outcome.
Concomitant presence of DSA in CAABMR cases is associated with poorer kidney graft survival, particularly if non-adherence is also documented. Histological phenotype in DSA (+)/non-adherent cases show a simultaneous cellular and antibody-mediated pattern of injury, with higher interstitial of inflammation and acute humoral scores. Additionally, ah score was significantly reduced in these patients, showing arteriolar under-hyalinosis correlation with under-immunosuppression and, importantly, correlated inversely with graft failure. No anti-rejection treatment strategy correlated with an improved graft outcome.
