Factors Influencing Deceased Donor Consent Rates in Cape Town, South Africa
David Thomson1, Hloni Bookholane4, Tinus Du Toit1, Fiona McCurdie2, Luke Steenkamp2, Lousie Human3, Lettie Prins3, Alexia Michaelides3, Elmi Muller1.
1Department of Surgery, University of Cape Town, Cape Town, South Africa; 2Transplant Coordinator, Groote Schuur Hospital , Cape Town, South Africa; 3Transplant Coordinator, Netcare Private Hospital, Cape Town, South Africa; 4Medical Undergraduate, University of Cape Town, Cape Town, South Africa
Introduction: Deceased organ donation rates in South Africa are perceived to be very low with no published data available. There is no national coordinating body for transplantation activities and there are low levels of public awareness about donation. The Western Cape has transplant teams in the public and the private sector and a population of 5.8 million with 1.4 million accessing private health care.
Methods: A structured data collection sheet was completed by the transplant coordinators (2 state and 3 private) after every family approach for consent to organ donation from April 28th 2017 to 14th November 2017. Family demographics, circumstances of the approach to the family, and various key points in the transplant coordinator discussion were recorded and analysed in all cases whether consent was granted or refused. 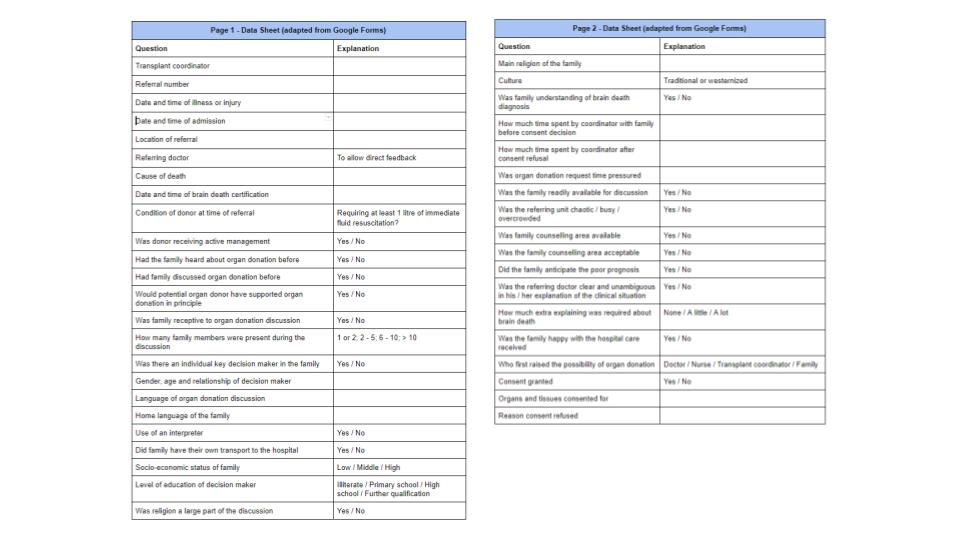
Results and Discussion: A total of 52 families were approached for consent with 48 in the public sector and only 4 in the private sector. The consent rate was low at 17.3%. There was a 100% refusal rate in the private sector. The condition of the donor at the time of referral was poor with only 52.9% still being actively managed by the treating team. Most potential donors (75%) required at least a litre of immediate fluid resuscitation at the time of initial assessment.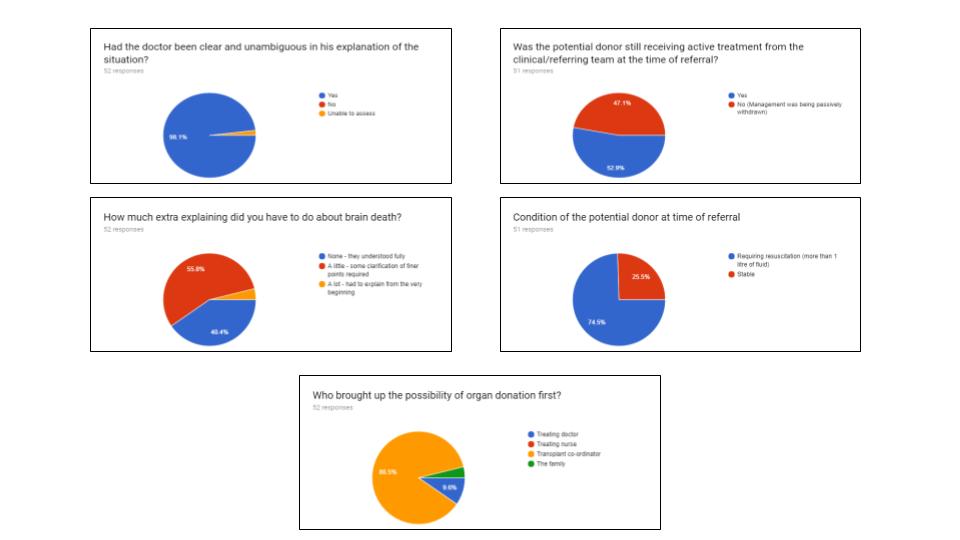
The majority of referrals (75%) came from trauma or casualty units with only 13 (25%) being referred from an Intensive Care Unit. All private sector referrals were in an Intensive Care Unit.Traumatic brain injury was the most frequent cause of death (75%).
Family discussions were often large with 25% involving between 6 - 10 people and 21.2% involving more than 10 people. A group decision about donation was made in 71.2% of cases. Only 51.9% of families had heard about organ donation prior to being approached and only 9.6% had discussed organ donation as a family. No potential donor was a registered organ donor. In most cases (84.6%) the family was receptive to the organ donation discussion.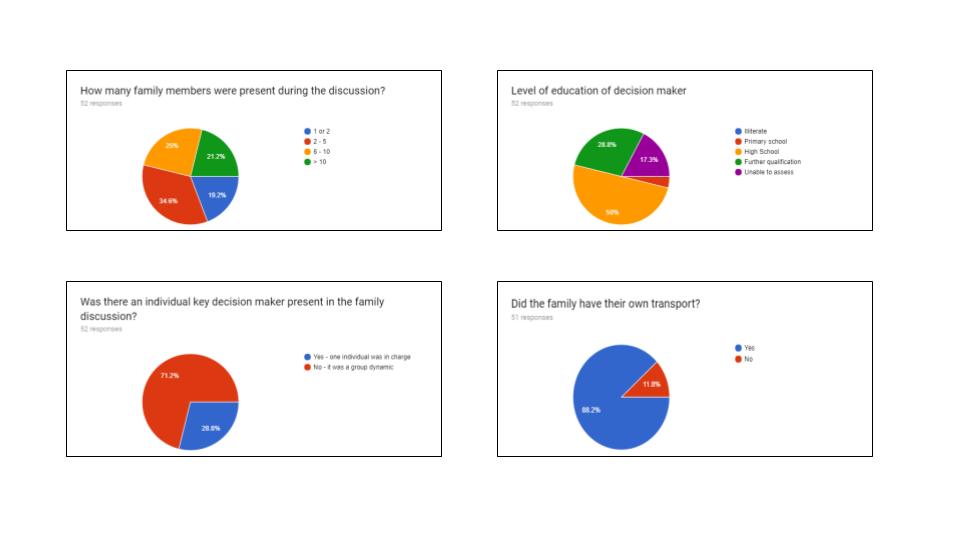
The consent discussion was held in English 86.5% of the time but for 35.3% of families their home language was Afrikaans and for 23.5% it was isiXhosa.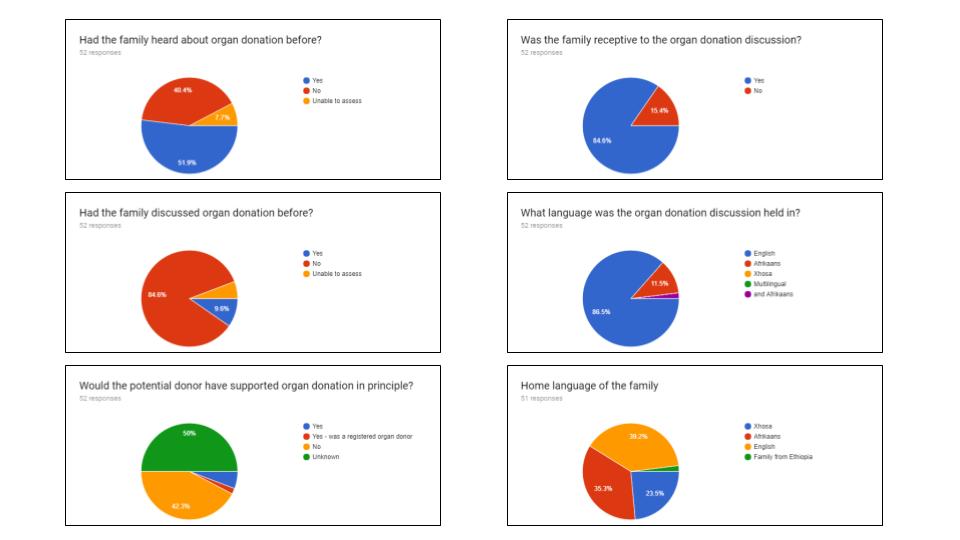 An interpreter was used in 1 case. The most commonly cited reasons for not supporting organ donation were against my religion (32.6%) and against my culture (25.6%). A religious leader was involved in 2 cases.
An interpreter was used in 1 case. The most commonly cited reasons for not supporting organ donation were against my religion (32.6%) and against my culture (25.6%). A religious leader was involved in 2 cases.
Conclusion: Consent rates were low. Despite most families not being aware of organ donation most families were receptive to discussions around organ donation. Decision making was often made by a large family group. Many areas for improvement were identified by this study: increased public awareness about deceased donation, improved donor management, better access to ICU, improving the number of referrals and engagement with religious and cultural leaders.
