Evaluation of Enhanced Recovery Program in Liver Transplanted Patients: Can We Beat the Benchmarks in Liver Transplantation?
Benny Wang1, Antonio Romano1, Felicia Kjaernet1, Carl Jorns1, Gunnar Soderdahl1, Bo-Göran Ericzon1, Greg Nowak1.
1Transplantation, Karolinska University Hospital, Stockholm, Sweden
Introduction: The recently proposed benchmarks in liver transplantation have shown, despite excellent patient and graft survival, a not satisfactory postoperative course in terms of length of hospital stay (LOS) and high rates of complications. Enhanced recovery programs (ERP) are widely used across different surgical disciplines, and have shown reduced LOS and morbidity. However, its feasibility in the field of liver transplantation has not been established. Herein, we conducted this study to investigate the potential benefits of ERP and whether its application can beat the current benchmarks in liver transplantation.
Methods: We retrospectively studied all adult liver transplanted patients (≥18 years old) that followed our ERP between January 2016 and June 2017. Patients were excluded from ERP due to following reasons: ICU before transplant, encephalopathy grade III-IV before transplant, complicated surgery, combined organ transplantations, ICU stay >2 days post-transplant and acute re-transplantation. Outcomes were compared with patients who followed a conventional postoperative care pathway meeting the benchmark criteria as defined in the study by Muller et al between January 2010 and December 2015. All patients had a minimum follow up time of 3 months. Endpoints were LOS, readmissions within 30 and 90 days, number and grade of post-transplant complications according to the Clavien-Dindo classification within 1 year, biliary complications within 1 year, patient survival and graft survival.
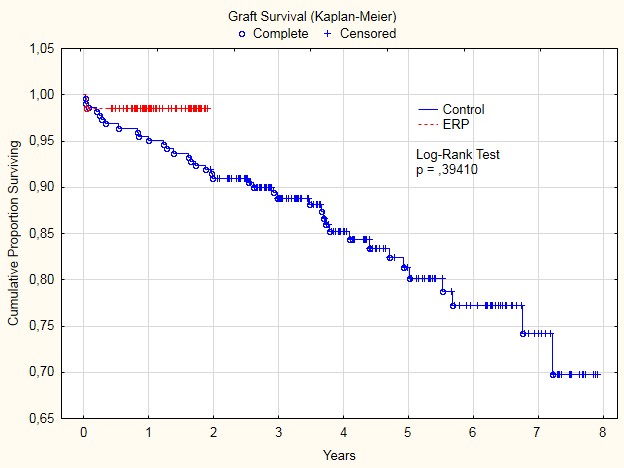
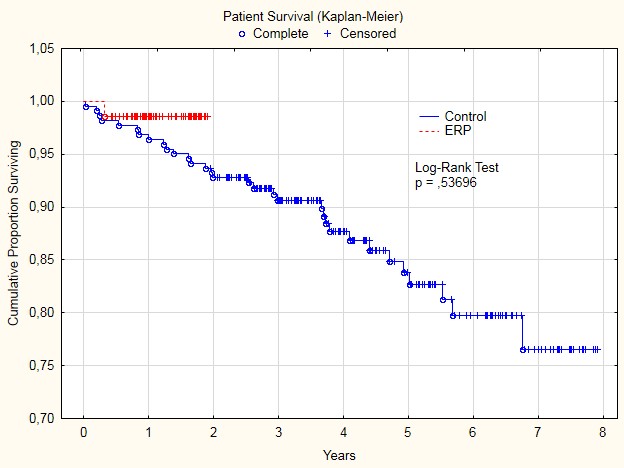
Results: 69 out of 115 (60%) patients followed ERP and were included to the study group. 222 out of 405 (55%) patients met the benchmark criteria and were included to the control group. Donor and recipient demographics did not differ between the two groups. The ERP group had lower incidence of post-transplant complications (69,0 % in ERP group vs 85,1 % in control group, P=0,011) and shorter median LOS (9 days in ERP group vs 13 days in control group, P<0,001). There were no differences in readmission rate within 30 and 90 days, postoperative complications, patient survival and graft survival.
Conclusion: Enhanced recovery programme can improve the postoperative course after liver transplantation by reducing post-transplant complication and length of hospital without having any adverse effects. These results may have important implications in refining the postoperative care and improve the current benchmarks in liver transplantation.
|
|
ERP group (n=69) |
Control group (n=222) | P-value |
| LOS | 9 (IQR 8-11) | 13 (IQR 11-17) | <0,001 |
| Readmission within 30 days (%) | 15 (22,0) (m=1) | 56 (25,8) (m=5) | NS |
| Readmission within 90 days (%) | 20 (29,0) | 87 (39,9) (m=4) | NS |
| N with post-transplant complications (%) | 29 (69,0) (m=27) | 149 (85,1) (m=48) | 0,011 |
| N with complication ≤ grade IIIa within 1 year (%) | 16 (38,1) (m=27) | 87 (50,0) (m=48) | NS |
| N with complication ≥ grade IIIb within 1 year (%) | 13 (30,1) (m=27) | 62 (35,6) (m=48) | NS |
| Biliary complication within 1 year (%) | 4 (9,5) (m=27) | 31 (17,7) (m=48) | NS |
m= number of patients with missing data, n = number of patients.