Intestinal Transplantation: from Rescue Therapy to Standard of Care for Intestinal Failure?
Emilio Canovai1,2, Laurens Ceulemans1,2, Ilse Hoffman3, Gert de Hertogh1,4, Martin Hiele1,5, Mauricio Sainz-Bariga1,4, Diethard Monbaliu1,2, Ina Jochmans1,2, Tim Vanuytsel1,5, Jacques Pirenne1,2.
1 Leuven Intestinal Failure and Transplantation Center, University Hospitals Leuven, Leuven, Belgium; 2Abdominal Transplant Surgery, University Hospitals Leuven, Leuven, Belgium; 3Paediatrics, University Hospitals Leuven, Leuven, Belgium; 4Pathology, University Hospitals Leuven, Leuven, Belgium; 5Gastroenterology and Hepatology, University Hospitals Leuven, Leuven, Belgium
Introduction: Intestinal Transplantation (ITx) is standard treatment for intestinal failure patients with life-threatening complications of home parenteral nutrition (HPN). Furthermore, refractory diffuse portomesenteric thrombosis is a growing indication for multivisceral transplantation (MVTx). Traditionally, ITx has had lower long-term survival compared to other solid-organ transplants (due to higher risk of rejection /infection) and compared to HPN. This often leads to late referral for ITx when malnourishment and vascular access problems increase perioperative risks.
Aim: To study the results of a single-center cohort of ITx patients and discuss possible change/evolution in indications for ITx.
Methods: A retrospective analysis of a prospectively maintained database of a single-center cohort of ITx patients transplanted from 2000-2017 was performed. Demographics, indication, graft type, rejection episodes, survival, costs versus HPN and quality of life were recorded.
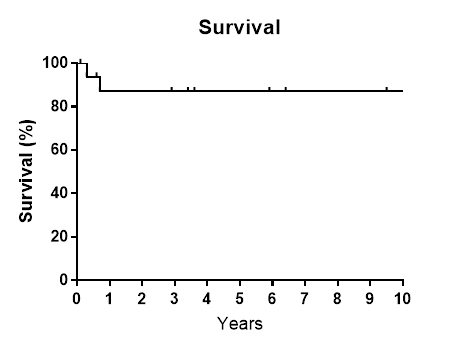
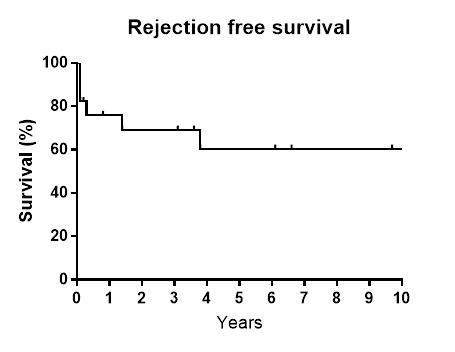
Results: In this period, 17 patients (13 adults (median age 43 years) and 4 children (median age 6 years) were transplanted. The majority of indications were short bowel syndrome and diffuse portomesenteric thrombosis. Seven patients underwent isolated ITx, 5 combined Liver-ITx and 4 multivisceral transplantations. Patients were treated according to a previously described immuno-suppressive (basiliximab, tacrolimus, azathioprine, steroids) and immunomodulatory protocol (Donor-specific blood transfusion & interventions aimed at reducing inflammation and endotoxin load) (Ceulemans et al. Am J Tx 2016). Cold ischemia times were kept short by synchronizing donor and recipient operations (median: 5.35 hrs.). Parenteral nutrition was stopped before discharge in all survivors. 10-year patient survival was 87%. Median Karnofsky score amongst survivors was 90-100%. There were 10 acute rejection episodes in 6 patients which all resolved with medical treatment. One patient developed sclerosing mesenteritis which was treated with everolimus. Two patients died in the first year after ITx due to invasive aspergillosis infections. One patient died more than 11 years after ITx due to NSAID induced enteropathy. The first year cost of ITx was more expensive than HPN (€185.662 vs 59.524). However, in the subsequent year ITx patients became far cheaper compared to HPN (Y1: €44.893, Y2: €18.976).
Conclusions: In this series, results of ITx compare favorably to HPN and other solid organ transplants. Diffuse splanchnic thrombosis is an expanding indication for MVTx. Excellent long-term results in addition to cost effectiveness and excellent quality of life indicate that ITx may be offered earlier in the course of intestinal failure.