
Isolated V-Lesion Early after Kidney Transplantation May Not Truly Represent a Rejection
Mariana Wohlfahrtova1,2, Petra Hruba2, Marek Novotny1, Jiri Klema3, Zdenek Krejcik5, Viktor Stranecky4, Eva Honsova6, Petra Vichova7, Ondrej Viklicky1,2.
1Department of Nephrology, Institute for Clinical and Experimental Medicine, Prague, Czech Republic; 2Transplant Laboratory, Institute for Clinical and Experimental Medicine, Prague, Czech Republic; 3Department of Computer Science, Czech Technical University in Prague, Prague, Czech Republic; 4Institute of Inherited Metabolic Disorders, 1st Faculty of Medicine Charles University and General Faculty Hospital, Prague, Czech Republic; 5Institute of Haematology and Blood Transfusion, Prague, Czech Republic; 6Department of Clinical and Transplant Pathology, Institute for Clinical and Experimental Medicine, Prague, Czech Republic; 7Department of Immunogenetics, Institute for Clinical and Experimental Medicine, Prague, Czech Republic
Background: Acute vascular rejection (AVR) is known to be a negative prognostic factor for kidney allograft survival. However, a role of early isolated v-lesion (IV) defined as intimal arteritis with minimal tubulointerstitial inflammation (TI) is unclear. While some authors believe in hidden ischemic/reperfusion injury, others are convinced of its rejection origin. However, current Banff classification assesses IV as type 2 or 3 of acute T-cell or antibody mediated rejection. To help resolve if IV truly represents acute rejection, molecular profiling of IV and T-cell mediated vascular rejection (TCMRV) was performed.
Materials and Methods: Gene expression profile of early IV (n=6) and TCMRV (n=4) within 1st month after kidney transplantation was compared using microarrays (Illumina Human HT-12 v4 Expression BeadChips). Differentially expressed genes were defined as those with fold change > 2 and adjusted p-value <0.05 corrected for multiple testing. The enrichment of dysregulated genes in biological processes was analysed using DAVID database.
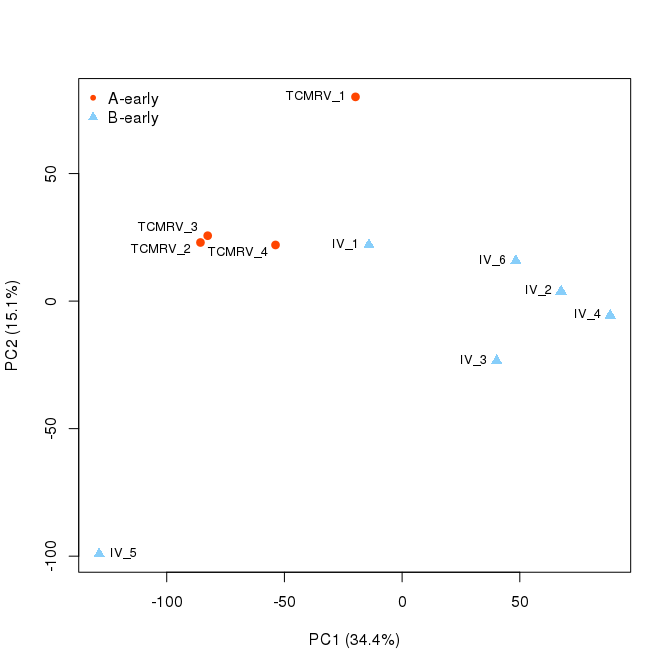
Results:Using microarray-based gene expression profiling in a training set of patients (n= 10), we identified 288 upregulated and 22 downregulated genes in early TCMRV compared to IV (Fig.1).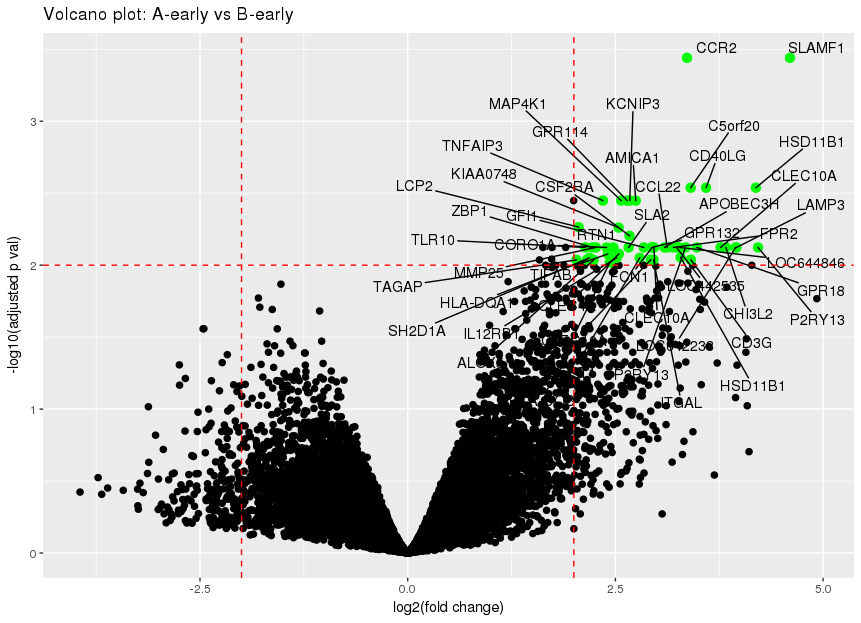 These dysregulated genes were primarily associated with T and B cell activation, costimulation, differentiation, receptor signalling pathway, antigen processing and presentation indicating higher innate and adaptive immune response and inflammation in early TCMV biopsies (Table 1). Hierarchical clustering (Fig. 2) and principal component analysis (Fig. 3) applied to the whole microarray data indicated a clear distinction in kidney allografts with TCMRV and IV.
These dysregulated genes were primarily associated with T and B cell activation, costimulation, differentiation, receptor signalling pathway, antigen processing and presentation indicating higher innate and adaptive immune response and inflammation in early TCMV biopsies (Table 1). Hierarchical clustering (Fig. 2) and principal component analysis (Fig. 3) applied to the whole microarray data indicated a clear distinction in kidney allografts with TCMRV and IV.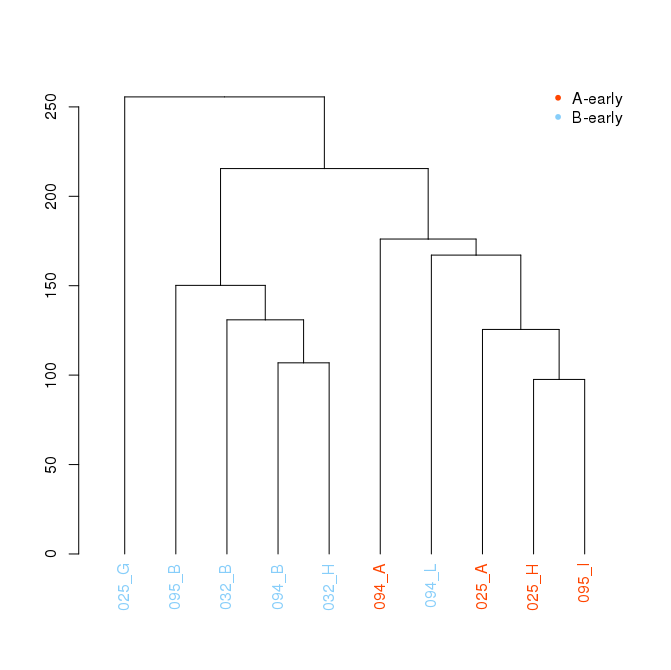
 Our findings were verified in an independent validation set of patients (n = 20) using RT-qPCR and confirmed increased expression of genes associated with immunity and inflammation in TCMRV.
Our findings were verified in an independent validation set of patients (n = 20) using RT-qPCR and confirmed increased expression of genes associated with immunity and inflammation in TCMRV.
Discussion: Our study provides a resource for better understanding the origin of isolated v-lesion and are in agreement with recent literature evidence which shows that intimal arteritis has probably less importance in diagnostics of TCMR than TI infiltrate. Furthermore, absence of TI inflammation in biopsies with IV makes TCMRV very unlikely (Reeves et al., Am J Transplant 2016).
Conclusion: Early isolated v-lesion has transcriptional profile of immune injury of significantly lower extend compared to T-cell mediated vascular rejection. According to this genome-wide transcriptome analysis early IV may feature non-rejection phenotype. Our findings call for reassessment of current histopathology classification which considers intimal arteritis to be at least grade 2 of T-cell mediated rejection irrespective of TI inflammation. Although more emphasis is placed in research on detrimental humoral phenotype, larger investigation is warranted to provide insight into cellular phenotype of AVR after kidney transplantation.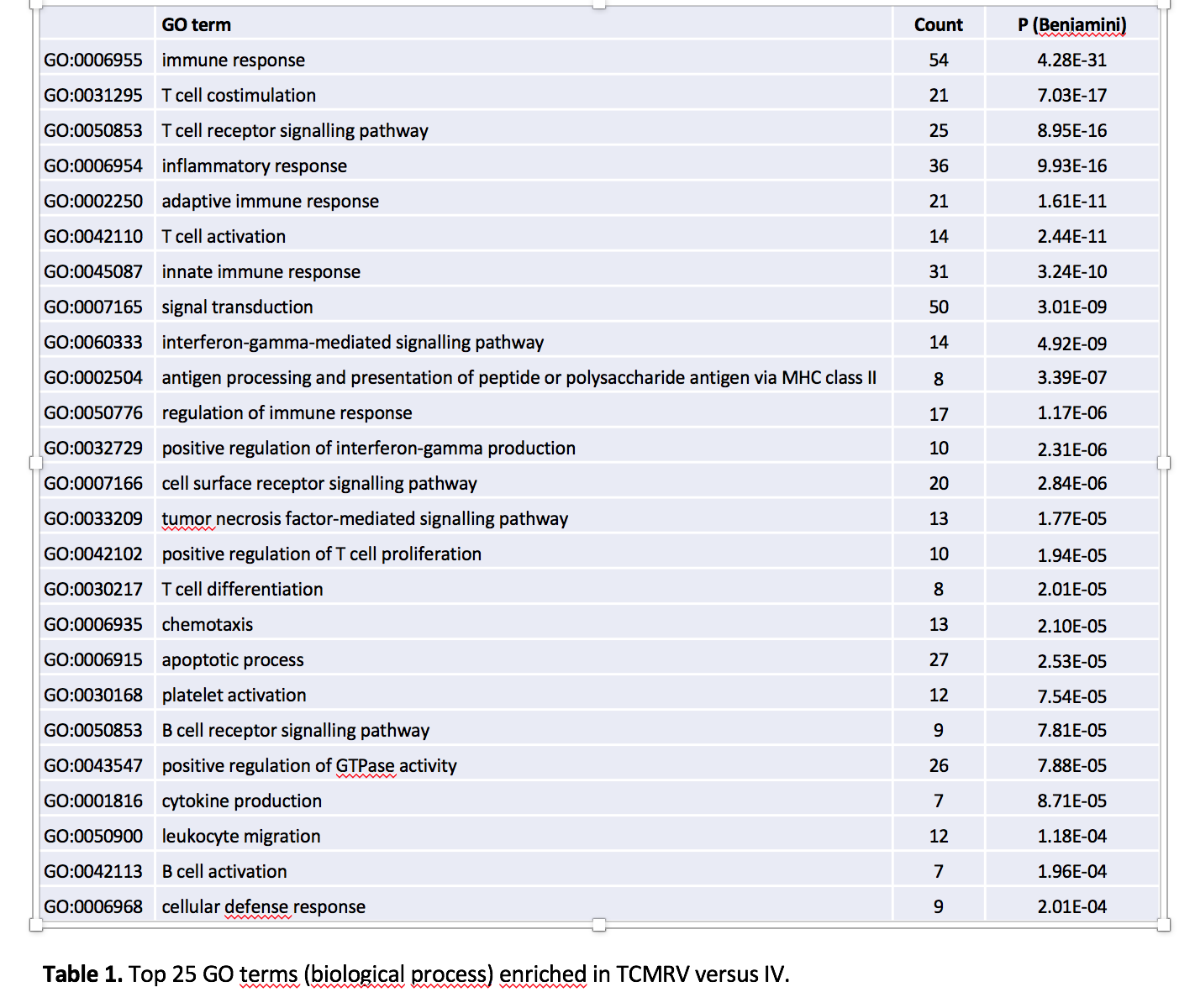
Supported by Ministry of Health of the Czech Republic, grant nr. 15-26519A and 17-29992A..
