Influence of Hypomagnesemia on New-Onset Diabetes After Kidney Transplantation
Korntip Phonphok1, Tin Duong1, Marina Habib1, Arpan Shah1, Nakul Datta1, Suphamai Bunnapradist1.
1Medicine-Nephrology, UCLA, Los Angeles, CA, United States
Introduction: Hypomagnesemia is commonly seen early after kidney transplantation (KT). Several studies have shown hypomagnesemia is an independent risk of new-onset diabetes after transplantation (NODAT) and may have the faster development of NODAT than normomagnesemia. We would examine hypomagnesemia as well as the reduction in serum magnesium (SMg) levels post-transplant on the risk of NODAT within the first year after KT.
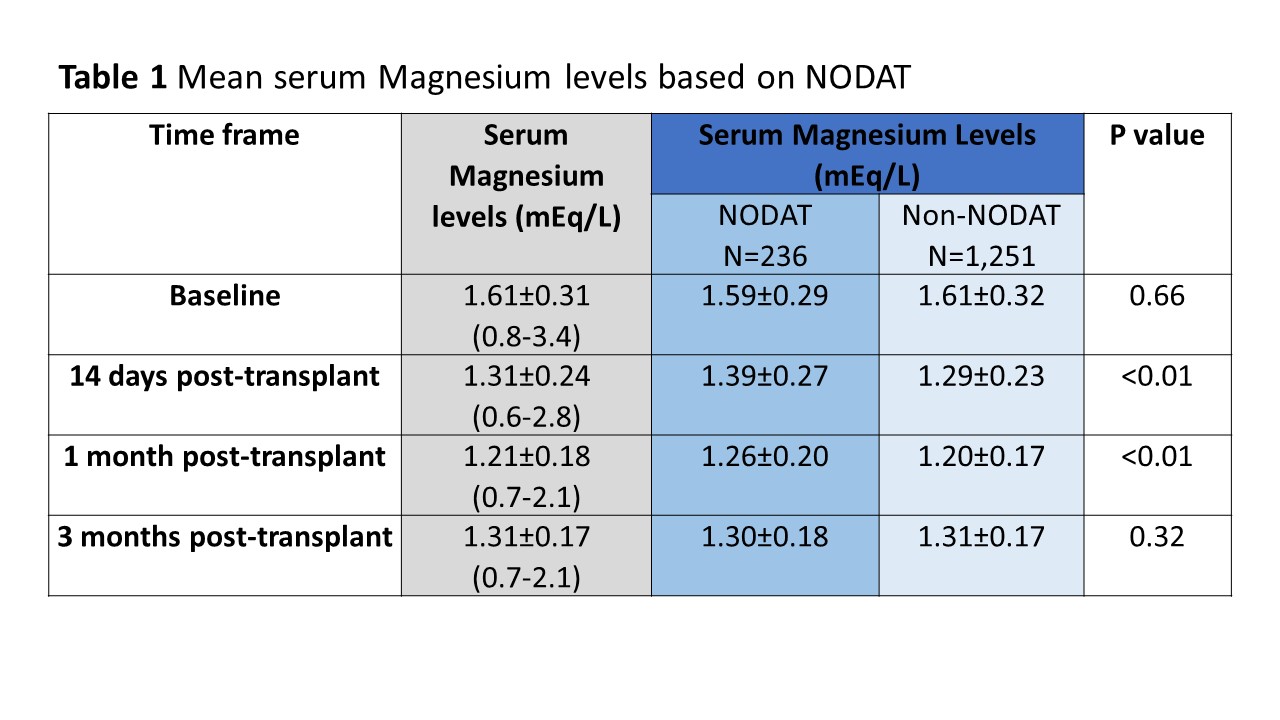
Materials and Methods: We examined 3,014 kidney transplant recipients from January 1, 2006, to May 31, 2016. Patients having serum magnesium levels at baseline, defined as 1-day pre-transplant, and post-transplant period at 14 days, 1 month, and 3 months were included. Patients with a history of pre-transplant diabetes were excluded from this study. NODAT was identified if patients met ADA criteria within 1-year post-transplant. We examined the mean of SMg levels and compared between NODAT and non-NODAT patients by using Wilcoxon rank-sum (Mann-Whitney) test. Patients were also divided into low Mg (SMg <1.4 mEq/L) and normal Mg (SMg≥1.4 mEq/L) group. We also analyzed the risk of NODAT and time to develop NODAT between groups using cox-proportional model.
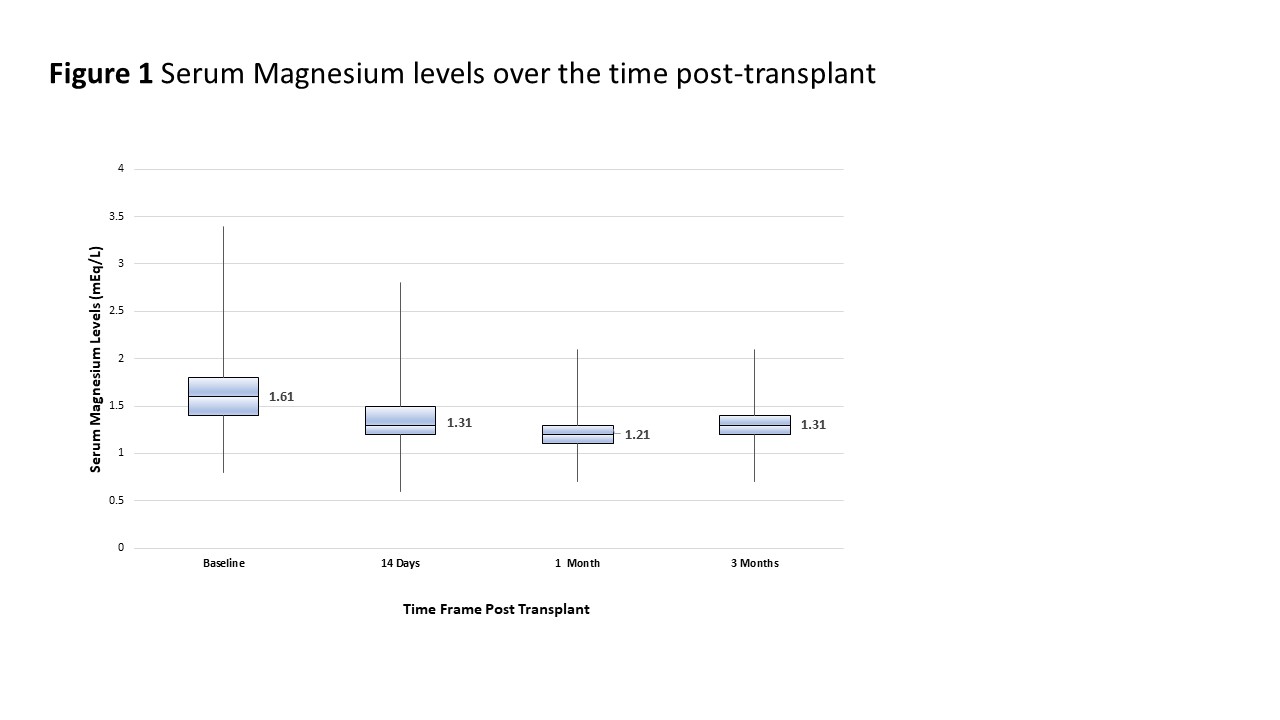
Results: 801 (26.58%) patients with a history of pre-transplant diabetes were excluded. A total of 1,487 patients had complete data, among these 236 (15.87%) of them developed NODAT within one-year post-transplant. SMg levels had decreased after KT and went to the lowest levels at 1 month post-transplant (Table 1, Figure 1). Mean SMg level at 14 days and 1 month post-transplant of NODAT patients were greater than non-NODAT patients (Table 1). We found that 1,258 patients (84.60%) had decreased in SMg levels at 1 month and the mean decreasing value was 0.49 mEq/L. Using 0.5 mEq/L as a cut-off decreasing value, patients with lesser reduction in SMg showed association with NODAT risk (p=0.01). As seen in Table 2, at 1 month post-transplant, normomagnesemic patients had greater risk to develop NODAT (30.71% vs. 14.33%; p<0.01) but had a similar time frame to develop NODAT (p=0.11).
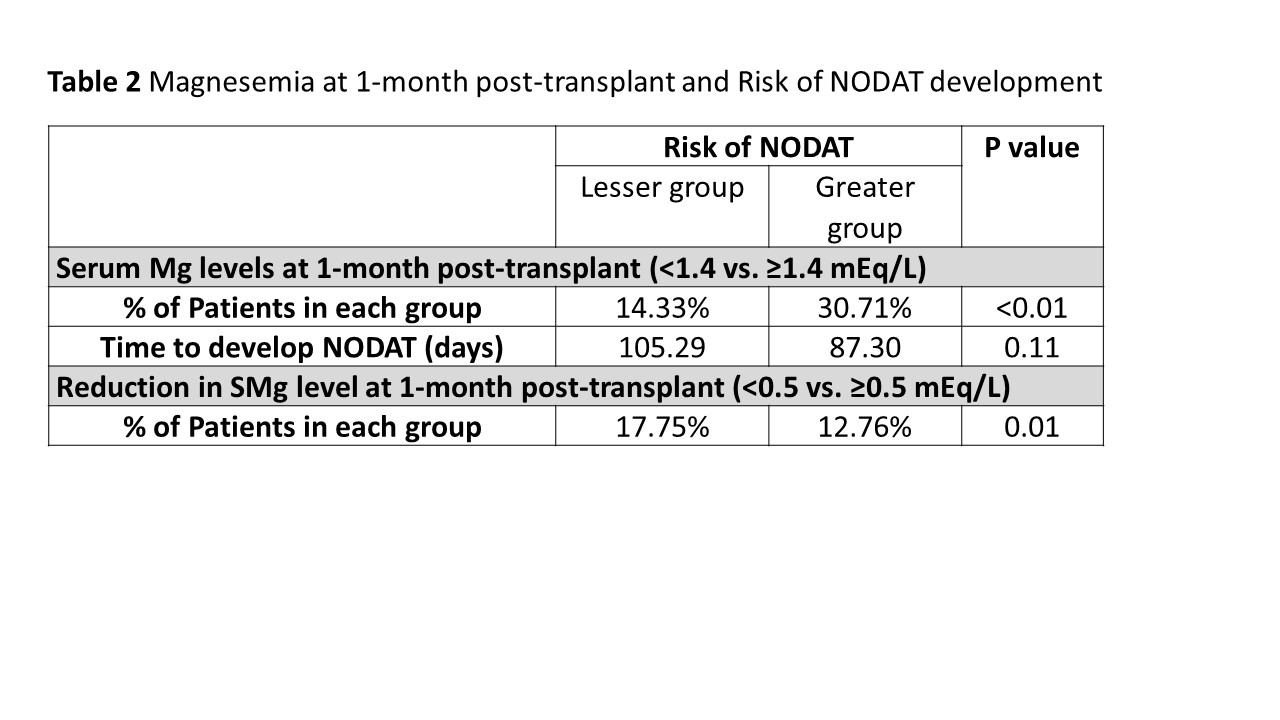
Conclusions: Majority of patients had decreased SMg levels after KT. However, we did not find independent associations between hypomagnesemia and risk of NODAT. A greater reduction in SMg levels did not show an additional risk of NODAT. On the other hand, post-transplant normomagnesemic patients were more likely to have NODAT. Future studies included various factors affecting NODAT should support evidence how magnesium may impact on NODAT.
