Neutrophil-Macrophage Communications via Inflammasome Pathway Induced Graft Injury after LDLT
Hui Liu1, Wai Ho Oscar Yeung1, Jiang Liu1, Xiao Bing Liu1, Tak Pan Kevin Ng1, Yuen Yuen Alice Ma1, Chung Mao Lo1, Kwan Man1.
1Surgery, The University of Hong Kong, Hong Kong, P.R. China
Introduction The shortage of donors urged clinical practitioners to expand the selection criteria to fatty grafts, which are more prone to liver graft injury. Inflammasomes are responsible for acute-phase inflammation after living donor liver transplantation (LDLT). Increased neutrophils and macrophages are observed in liver grafts. Despite the roles of individual immune cell, the regulation of inflammasomes on neutrophil-macrophage communications and the effects on macrophage phenotype switch was little known during liver graft injury.
Materials and Methods The associations among inflammasomes, neutrophils and pro-inflammatory (M1) macrophages during liver graft injury were investigated in liver biopsies from LDLT patients and rats with orthotopic liver transplantation model using small-for-size graft. The mechanism of inflammasomes as the link role on neutrophil-macrophage communications and the switch of macrophage phenotypes were further examined both in mouse hepatic ischemia/reperfusion injury model with major hepatectomy and in vitro neutrophil-macrophage co-culture system.
Results and discussion The increase of intragraft NLRP3 inflammasomes in neutrophils and accumulated M1 macrophages were associated with deteriorated liver function (elevated ALT and AST) in fatty graft of LDLT patients at 2 hours after reperfusion. Intragraft NLRP3 and NLRC4 inflammasomes were also significantly raised at acute phase in rat liver transplantation model using small-for-size fatty graft (Figure 1).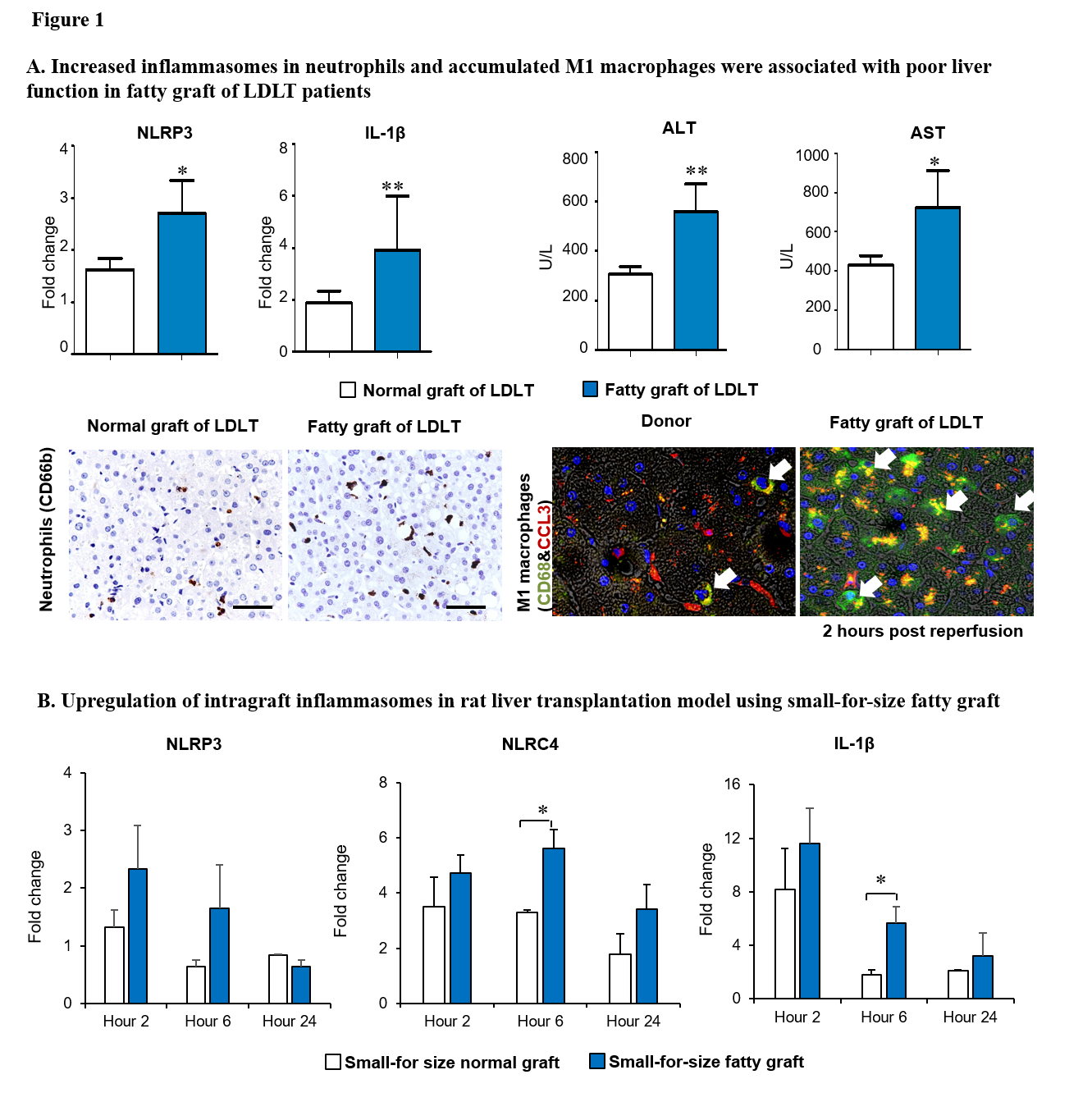 In our mouse ischemia/reperfusion injury model with major hepatectomy, the upregulation of hepatic NLRP3 inflammasomes in neutrophils at Hour 2 led to more macrophages infiltration at Hour 6 after reperfusion. Through the co-culture of LPS-stimulated neutrophils with macrophages, the pro-inflammatory cytokines (IFN-γ, TNF-α and IL1β) were significantly upregulated while the anti-inflammatory receptor (IL-4R) was decreased in macrophages accompanied with the increase of NLRP3 inflammasomes in neutrophils (Figure 2).
In our mouse ischemia/reperfusion injury model with major hepatectomy, the upregulation of hepatic NLRP3 inflammasomes in neutrophils at Hour 2 led to more macrophages infiltration at Hour 6 after reperfusion. Through the co-culture of LPS-stimulated neutrophils with macrophages, the pro-inflammatory cytokines (IFN-γ, TNF-α and IL1β) were significantly upregulated while the anti-inflammatory receptor (IL-4R) was decreased in macrophages accompanied with the increase of NLRP3 inflammasomes in neutrophils (Figure 2).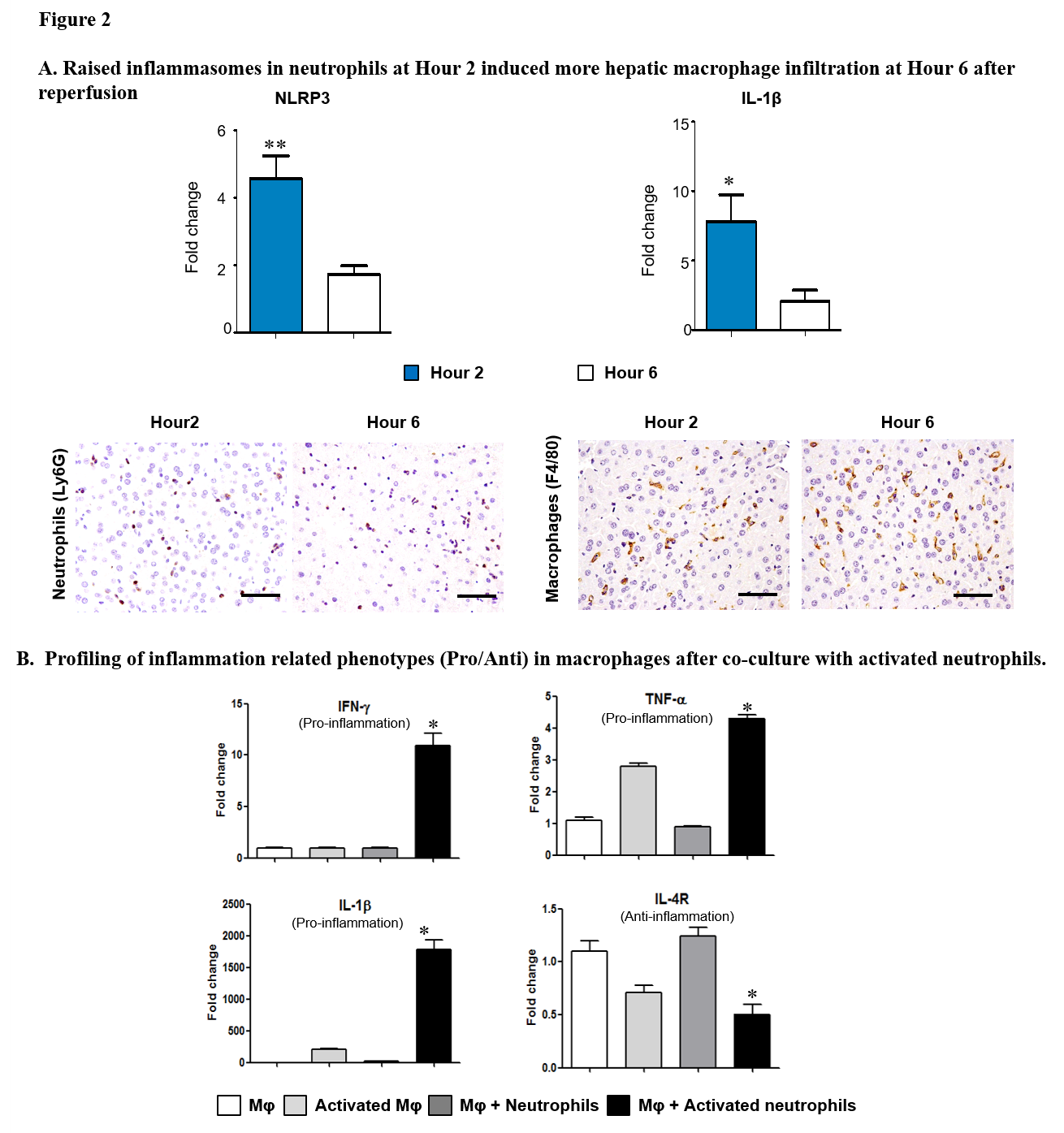 These results indicated that the activation of inflammasomes in neutrophils may prime the macrophages switching to M1 phenotype in liver graft injury.
These results indicated that the activation of inflammasomes in neutrophils may prime the macrophages switching to M1 phenotype in liver graft injury.
Conclusion The inflammasomes play a critical role in neutrophil-macrophage communications during liver graft injury after LDLT. The macrophages switching to M1 phenotype by inflammasome activation in neutrophils may be a key mechanism to initiate inflammation in liver graft injury.
