High Incidence of Anal Human Papillomavirus Infection in HIV-infected Solid Organ Transplant Recipients
Peter ChinHong1, Burc Barin2, Michael Berry1, Maria DaCosta1, Tere Darragh1, Lori Rosenthal3, Steve Bartlett4, Douglas Dieterich5, Fred Poordad6, Nicholas Nissen6, Mike Wong7, Peter Stock1, Joel Palefsky1.
1University of California, San Francisco, San Francisco, CA, United States; 2EMMES, Rockville, MD, United States; 3Columbia University, New York, NY, United States; 4University of Maryland, Baltimore, MD, United States; 5Icahn School of Medicine at Mount Sinai, New York, NY, United States; 6Cedars-Sinai Medical Center, Los Angeles, CA, United States; 7Beth Israel Deaconess Medical Center, Boston, MA, United States
Introduction: Infection with human papillomavirus (HPV), particularly high-risk types (HR-HPV), is an important cause of anogenital and head and neck cancers among both solid organ transplant recipients and HIV-infected patients. There is little data in dually-immunosuppressed HIV-infected transplant patients. We aimed to determine the prevalence, incidence and determinants of anal HPV infection in this population.
Methods: We enrolled HIV-infected patients in a multi-center study prior to transplantation. We collected baseline demographic, medical and behavioral information. We assessed anal HPV6/11/16/18/31/33/35/39/45/51/52/56/58/59 DNA by polymerase chain reaction at baseline, then at 6, 12 and 24 months post-transplant.
Results: Of 86 HIV-infected patients, 90% were male, 53% were men who had sex with men (MSM), 79% were white; 66% underwent liver and 34% kidney transplantation. The median age was 49 (IQR, 44-54). Nineteen percent reported a prior opportunistic infection, and 48% were Hepatitis C (HCV) infected. The median CD4+ prior to transplantation was 172 (IQR, 252-563). At baseline, 71% were infected with anal HPV and 38% were infected with HR-HPV. In a multivariable model, MSM behavior was associated with baseline HR-HPV (OR 3.0, 95% CI, 1.2-7.5). Among liver recipients, HCV infection was associated with lower HR-HPV prevalence (OR 0.2, 95% CI 0.1-0.7). Of those HR-HPV uninfected at the time of transplantation, 5% (95% CI, 1-28); 43% (95% CI, 25-66) and 67% (95% CI, 43-90) were infected by 6, 12 and 24 months post-transplant. 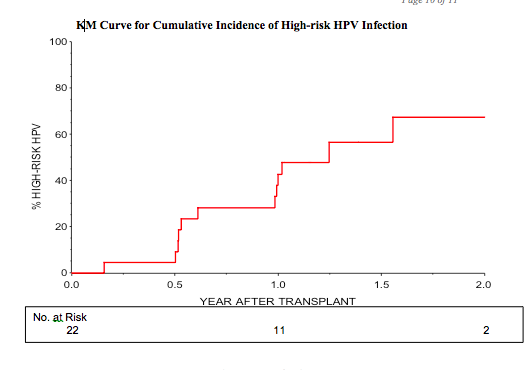
Conclusions: Anal HPV-infection is common in a pre-transplant population of immune reconstituted HIV-infected patients. Even if not present at the time of transplantation, by 2 years, 67% of patients had incident anal HR-HPV detected. Efforts to vaccine eligible patients prior to transplantation and anal cancer screening programs should be prioritized.
National Institues of Allergy and Infectious Diseases (AI052748).
