Retransplantation after Living Donor Liver Transplantation: Analysis of Data from the A2ALL Study
Garrett R Roll MD1, Hillary Braun1, Josh D Grab MS1, Jennifer L Dodge MPH1, Shareef M Syed MD1, Chris E Freise MD1, John P Roberts MD1, Nancy L Ascher MD, PhD1.
1Surgery, University of California, San Francisco, San Francisco, CA, United States
Introduction: Living donor liver transplant (LDLT) is associated with a higher incidence of post-transplant vascular and biliary complications, however it is also known that graft and patient survival after LDLT is similar to graft and patient survival following deceased donor liver transplantation (DDLT). Outcomes for retransplantation (reLT) after LDLT are not well understood; this study aimed to review the need for reLT following LDLT using data from the Adult to Adult Living Donor Liver Transplantation Study (A2ALL).
Materials and Methods: Demographics and outcomes of donors and recipients in the A2ALL cohort who underwent LDLT between April 1998 and January 2014 were reviewed. We compared recipients who underwent LDLT followed by reLT to recipients that underwent LDLT alone. Descriptive analysis was performed using Wilcoxon rank sum and chi-squared tests; patient survival was estimated using Kaplan-Meier methods and compared by the log-rank test.
Results: 1065 donor/recipient pairs were included in the analysis. 110 recipients (10.3%) required reLT following initial LDLT. reLT patients were predominantly male (65.5%) and Caucasian (94.5%), with a median (IQR) age of 49.2 years (40.9-57.3), median BMI of 25 (23-28), and median MELD of 16 (12-20). The majority were right lobe recipients (93.6%) and related to their donor (59.1%). Compared with patients who underwent LDLT alone, reLT patients were slightly younger (49.2 vs. 52.8 years, p=0.001) and had a higher total bilirubin at the time of LDLT (3.1 vs. 2.6, p=0.02). The most common cause of graft failure was vascular thrombosis (47.8%) followed by primary graft failure (19.4%), other (13.4%), and recurrent hepatitis (10.4%). ReLT patients had a longer length of stay in the hospital (18 vs. 10, p<0.001) and ICU (3 vs. 1 days, p<0.001) after initial LDLT, and a greater number of complications (5 vs. 3, p<0.001). Patient survival after initial LDLT was significantly lower for reLT versus LDLT alone (p<0.001). Survival (95% CI) for reLT and LDLT patients, respectively, was 86.2% (78-92) vs. 91.6% (90-93) at 1-year, 63.5% (53-73) vs. 81.9% (79-85) at 5-years, and 44.1% (31-56) vs. 67.9% (64-72) at 10-years (Figure 1).
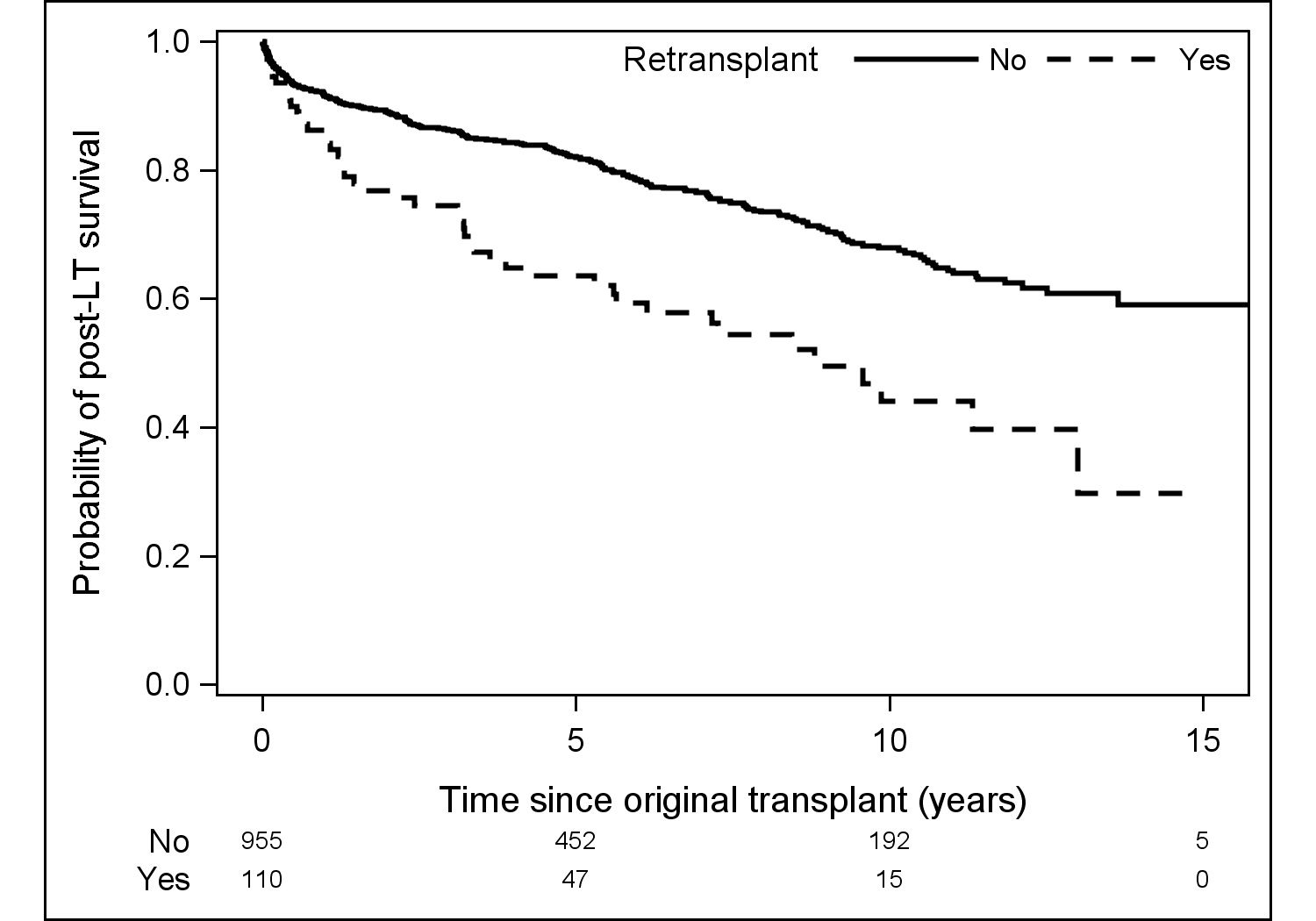
Discussion: In this cohort, vascular thrombosis and primary graft failure accounted for more than two thirds of all reLT after LDLT. In the United States, patients with these diagnoses may be listed as Status 1 and move to the top of the waitlist for deceased donor organs. However, reLT is associated with significant mortality and patients who require reLT following LDLT have significantly worse long-term survival post-transplant. ReLT poses a complex ethical and emotional dilemma for the transplant team, particularly in the case of reLT following LDLT.
Conclusion: Vascular thrombosis and primary graft failure are the most common indications for reLT following LDLT. ReLT after LDLT is associated with significantly worse patient survival at 5 and 10 years post-transplant.
