Perioperative Predictors of Acute Kidney Injury after Liver Transplantation and its Impact on Postoperative Outcome
Cristina J Lisbona1, Almudena L Vilchez Monge1, Inmaculada Hernández1, Ignacio Garutti1, Luis Olmedilla1, Consuelo Jiménez de la Fuente1, Matilde Zaballos1, José M Asencio2, José A López Baena2, Pablo Lozano2, José M Pérez-Peña1.
1Anesthesiology and Intensive Care, Hospital General Universitario Gregorio Marañón, Madrid, Spain; 2Surgery, Hospital General Universitario Gregorio Marañón , Madrid, Spain
Liver Transplantation Group.
Background and Goal of Study: Liver transplantation (LT) is the best treatment for patients with end-stage liver disease. It is a very complex surgery with high rates of morbidity and mortality. Acute kidney injury (AKI) is a common and serious complication after LT. The ability to early identify those patients at high risk of post-LT AKI is crucial, and could provide invaluable help for their proper management during and after LT surgery.
The aim of this study was to identify perioperative predictors of post-LT AKI and to assess the impact of AKI on postoperative outcome.
Materials and Methods: After approval by the Ethical Review Board, we conducted a prospective, single-center study of 242 consecutive adult patients undergoing LT between December 2010 and February 2017. Early AKI was defined according to KDIGO criteria (Kidney Disease Improving Global Outcomes). Serum creatinine was measured at baseline and up to 3 post-LT days. Patients with and without AKI were compared to identify perioperative predictors for this complication. Perioperative variables were collected, including demographic data, baseline creatinine, MELD and Child-Pugh scores, intraoperative hemodynamic data, and transfusion and fluid therapy. Length of intensive care unit (ICU) stay, hospital-stay, 30-day mortality and one-year mortality were studied as postoperative outcomes. For data analysis Man Whitney, Chi-square or Fisher exact tests were used.
Results and Discussion: The incidence of AKI at 72 h post-LT was 63.6% (154 patients). Only four variables were identified as predictors of post-LT AKI: higher recipient weight, hemodynamic data at end of surgery (cardiac index [CI] and renal perfusion pressure [RPP=mean arterial pressure minus inferior vena cava pressure]) and the amount of intraoperative colloid administration (table 1). The remaining pre- and intra-operative variables did not differ significantly between the two groups.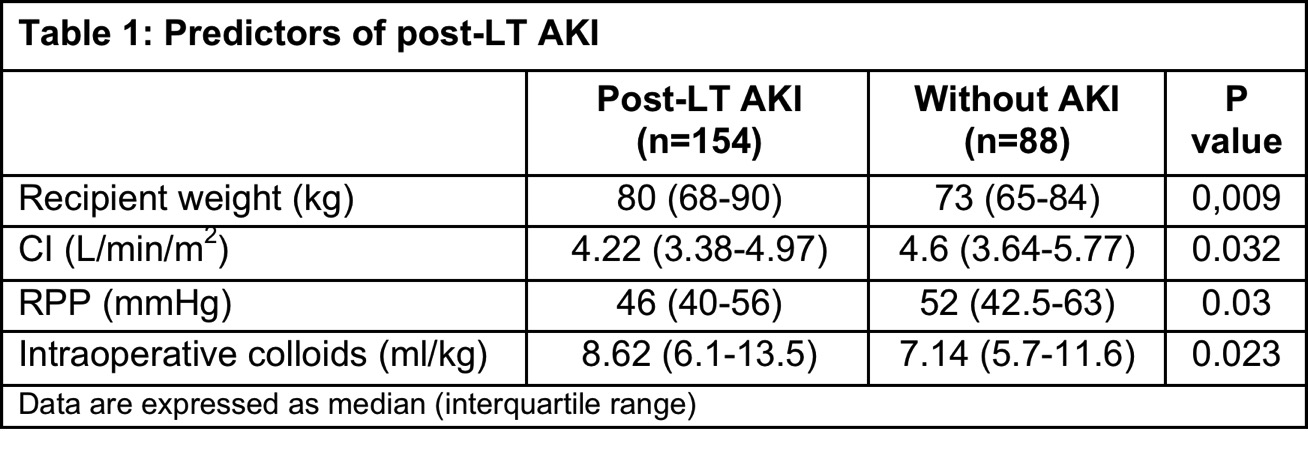
AKI after liver transplantation was associated with worse post-LT course, with longer ICU and hospital stay, and reduced 30-day and one-year survival (table 2).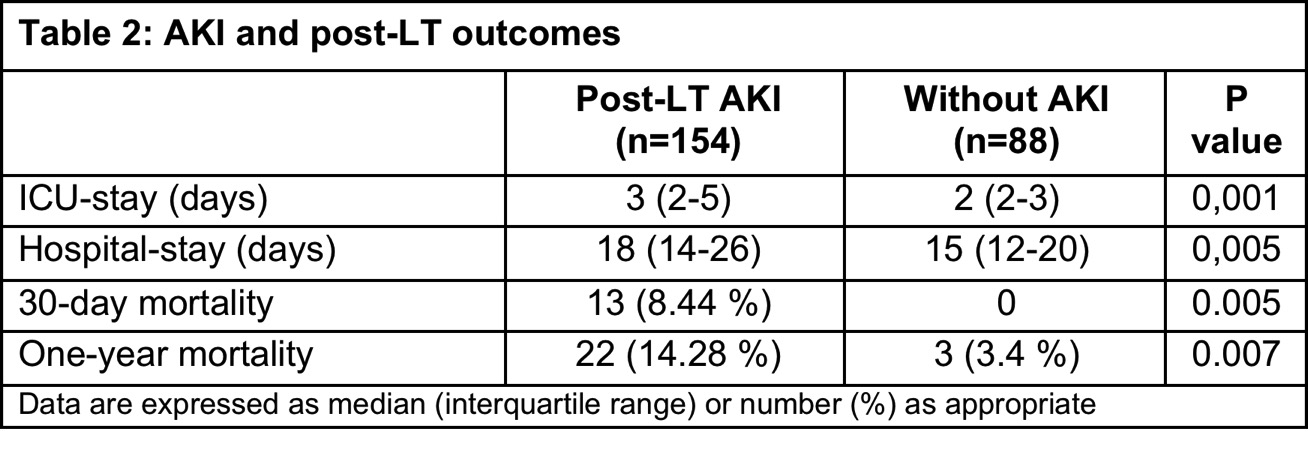
Conclusions: In patients undergoing LT there was a high incidence of early AKI. Development of AKI after LT was associated with a remarkably worse postoperative outcome. These results suggest that higher intraoperative colloid administration, lower CI and lower RPP had a negative impact on post-LT renal function. Thus, targeting modifiable risk factors, such as fluid therapy and hemodynamic derangements may reduce the incidence of AKI.
