Renal Transplant with Positive Virtual Crossmatch in Patients with High Immunological Risk
Sandra Elias1, Israel Gañan2, Milagros Fernandez-Lucas1, Cristina Galeano1, Sara Jimenez1, Ana Fernandez1, Jose Luis Castañer2, Fernando Liaño1.
1Nephrology, Hospital Ramón y Cajal, Madrid, Spain; 2Immunology, Hospital Ramón y Cajal, Madrid, Spain
Introduction: In the past few years the number of patients in the waiting list with anti-HLA antibodies has been increased. This makes it more difficult to find an appropriate immunological donor for these receptors. For that reason, we decided to perform in our hospital renal transplants with positive virtual crossmatch in certain patients.
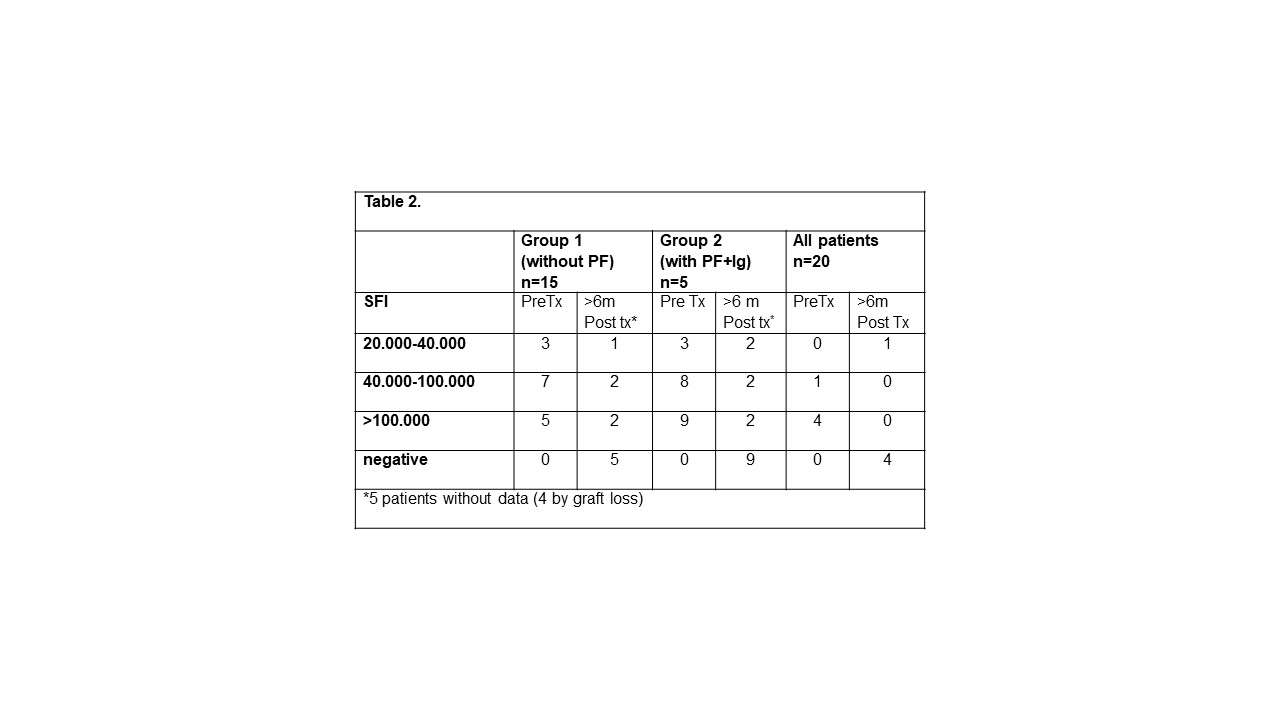
Materials and Methods: We analyzed the renal transplants performed in our hospital since October 2014 with positive virtual crossmatch and a specific donor antibody value greater than 20,000 SFI. A total of 27 patients have been included so far. In all cases the crossmatch test by cytotoxicity was negative at the time of transplantation. The induction treatment is with Anti-Thymocyte Globulin at doses of 4.5 mg/kg associated with corticoids, tacrolimus and mycophenolate mofetil. Since July 2016 the patients who have a sum of specific donor antibodies greater than 80.000 SFI or PRA greater than 98% receive a plasmapheresis cycle with human immunoglobulin, starting at day + 5 post-transplant. In this paper we present the clinical and immunologic data of patients who have completed 1 year of follow up.
Results: Of the 27 renal transplants performed with this protocol 20 patients have completed the 1 year follow up. The average age of the donors it is 64 years old and that of the recipients is 54-year-old. 5 patients received plasmapheresis and human immunoglobulin in immediate post-transplant prophylactically. In table 1 and 2 will expose the immunological data previous and posterior to renal transplant.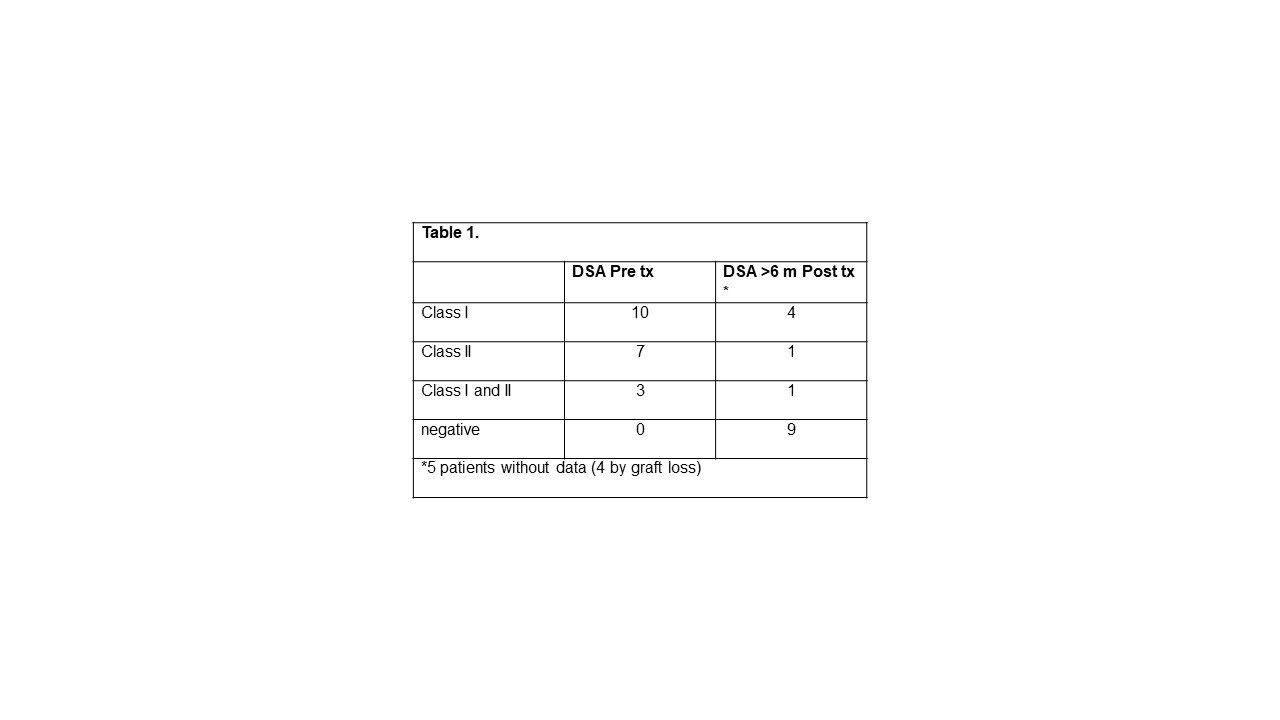
In terms of rejection cases, 5 humoral rejections were diagnosed (20%) of which 1 was the cause of the graft loss and the other 4 responded to the treatment. 4 of these patients were of the group without prophylaxis with plasmapheresis. The survival of the graft a year is 75% with 1 case of humoral rejection (5%) 2 for Pyelonephritis, 1 case of immediate thrombosis and one of death with a functioning graft. The patient's survival is 95% per year.
Discussion: Renal transplantation with specific donor anti-HLA antibodies is an option for hyperimmunized patients, as only one of the patients in our series lost the graft by humoral rejection. Greater number of patients required and more follow-up to obtain more conclusive data. The realization of plasmapheresis with human immunoglobulin after transplantation as prophylaxis, it seems to us a possibility to reduce the risk of humoral rejection in these patients. As a main complication of the increase in immunosuppression we found infections, which in 2 cases led to graft loss.
Conclusion: The renal transplant with virtual positive crossmatch is a valid option in patients with high antibody titers. Adding plasmapheresis in induction therapy may decrease the risk of humoral rejection.
