Re-Endothelialization of Liver Xenografts Utilizing Human Endothelial Cells
Wessam Hassanein1, Avraham Werdesheim1, Parth Patel1, Justin Brilliant1, E Bryan Buckingham1, Nicole Shockcor1, Cinthia Drachenberg2, Rolf N Barth1, John C LaMattina1.
1Surgery, University of Maryland, Baltimore, MD, United States; 2Pathology, University of Maryland, Baltimore, MD, United States
Introduction: Acute antibody mediated rejection due to preformed antibodies present in human serum remains a hurdle to successful xenotransplantation. Xenograft vascular endothelium represents the initial site of recipient immune exposure to xenoantigens. We hypothesized that biologically engineered liver xenografts after re-endothelialization of the vascular tree with allogenic endothelial cells has the potential to evade the recipient´s immune response against xenografts.
Methods: Adult rat livers were procured using aseptic technique (n=6). A novel protocol of selective de-endothelialization was developed utilizing 0.1% SDS perfusion for 15 min using our established bioreactor perfusion system. Treated grafts were examined by H&E staining and under immunofluorescent microscopy using rat specific anti-CD34 as endothelial cell marker. Human umbilical vein endothelial cells (HUVECs) were then introduced into the de-endothelialized livers, and perfused with culture media suplemented with appropriate growth factors. Grafts were kept for 3 days at 37C. Constructs were subsequently examined immunohistochemically for HUVECs using human specific anti-CD31.
Results: Livers treated with 0.1% SDS showed selective yet complete de-endothelialization compared to native liver (Fig 1A, 1B). The liver architecture remained intact and the majority of liver cells were viable following treatment. HUVECs were successfully engrafted onto the de-endothelialized rat liver vessels. This was confirmed by H&E and immunohistochemistry staining (Fig 1C, 1D).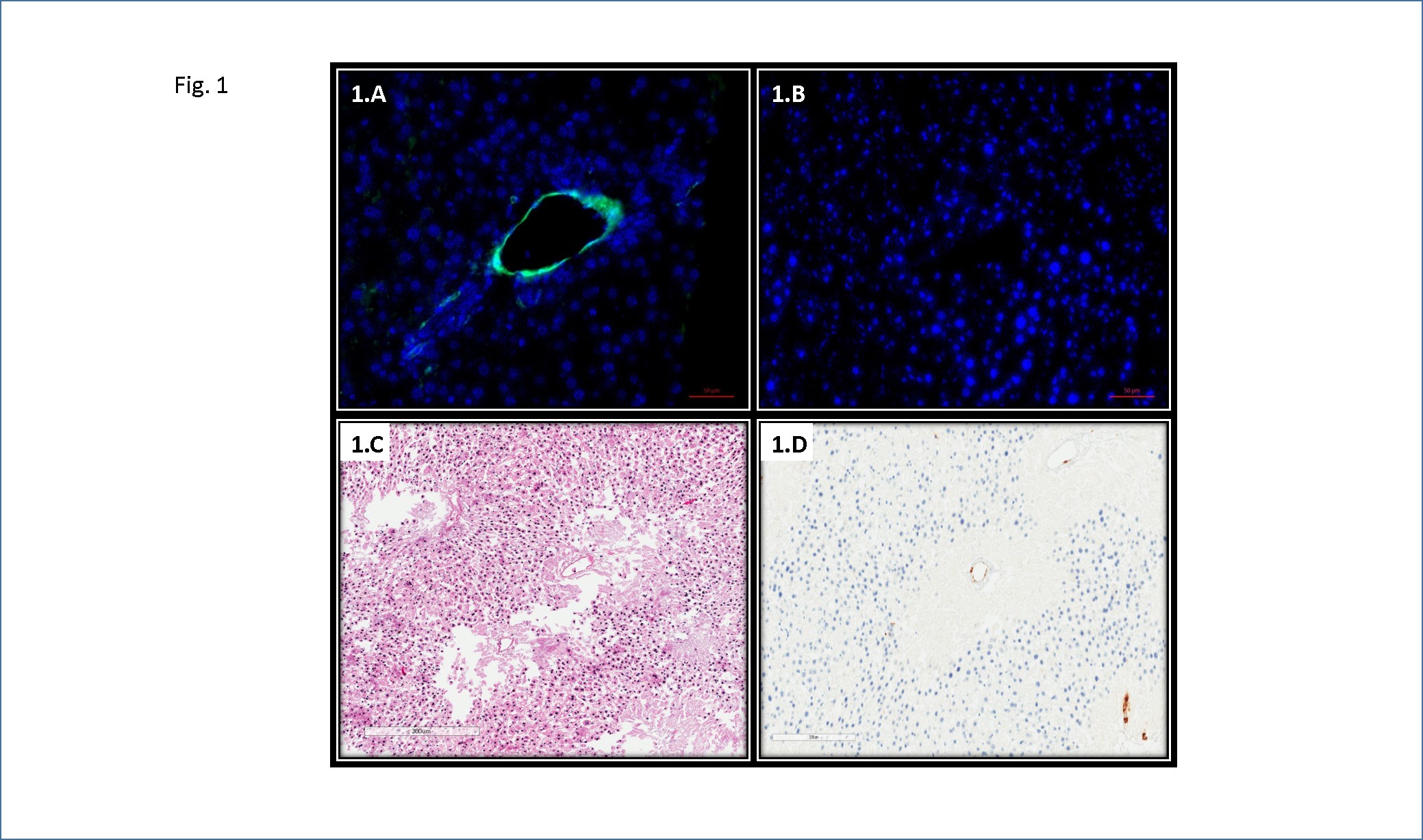
Conclusions: Selective de-endothelialization of rat livers was successful, and human cells could re-establish the xenograft vascular bed. This method demonstrates the ability to manipulate a key component of the immune response to xenogeneic antigen. Future experiments are directed at ex-vivo perfusion of the re-endothelilaized grafts with human blood.
