Transplantation Outcome after Pig to Mouse Intra-Portal Islet Transplantation
Jun-Seop Shin1,2,3,4, Il-Hee Yoon1,4, Byoung-Hoon Min1,3,4, Jong-Min Kim1,2,3,4, Jongwon Ha1, Sang-Joon Kim1, Chung-Gyu Park1,2,3,4.
1Xenotransplantation Research Center, Seoul, Korea; 2Institute of Endemic Diseases, Seoul, Korea; 3Cancer Research Institute, Seoul, Korea; 4Microbiology and Immunology, Seoul National University College of Medicine, Seoul, Korea
IIntroduction: Islet transplantation is considered a promising curative therapy for type 1 diabetes, but shortage of donor organ limits its wide adoption in the clinic. Porcine islets are potential source for allogeneic human islets, but the xenogenic immune responses remain a major hurdle for clinical application. Pig to mouse islet transplantation has been widely used to understand the xenogeneic immune responses to porcine islets, but its transplantation route has been different from that in clinical settings in most cases (kidney subcapsule vs. portal vein). Here we established clinically relevant intra-portal porcine islet transplantation model and examined the pattern of islet distribution and survival duration. The immune responses to porcine islets were compared with those from mouse allo-islet transplantation.
Materials and Methods:
Islet isolation and transplantation: Pig islets were isolated from designated pathogen-free SNU miniature pigs (n=3) using semi-automation method by Ricordi. Mouse islet was isolated from Balb/c mice using collagenase digestion and Ficoll gradient centrifugation. Porcine and murine islets were transplanted into the liver via a cecal vein into streptozotocin-induced diabetic C57B6 mice. Blood glucose levels were measured in tail vein by a glucometer.
Immunosuppression: Diabetic mice were intraportally transplanted with porcine islets (7500 IEQ/each, n=10) or allogeneic murine islets (500 IEQ/each, n=6). The half of the mice from each group were treated with MR1 antibody and the other half were vehicle treated. Anti-CD154 antibody (500 mg/mouse, MR1, BioXcell, Inc.) was i.p. injected at 0, 1, 3, 5, and 7 day post-transplantation.
Results: The number of the isolated porcine islets was 10,872±8,567 IEQ/g pancreas and purity was 90%. Upon porcine islet transplantation into the diabetic C57B6 mice, blood glucose levels were dropped to normoglycemia at 1 day post-transplantation, but increased to hyperglycemia over 250 mg/dl within 4~5 days regardless of MR1 treatment. In contrast, allogeneic murine islets maintained normoglycemia within 2 weeks and upon MR1 treatment they could prolong the normoglycemia over 100 days (Fig. 1).
Conclusion: In this study, the procedure for pig to mouse islet transplantation into the liver was established. Pig islets sustained only 4~5 days after intraportal transplantation into diabetic mice, whereas mouse islets maintained normoglycemia over 100 days upon T cell co-stimulation blockade treatment (MR1 antibody). This finding suggests that porcine islets have inherent survival inability in the liver upon intraportal islet transplantation.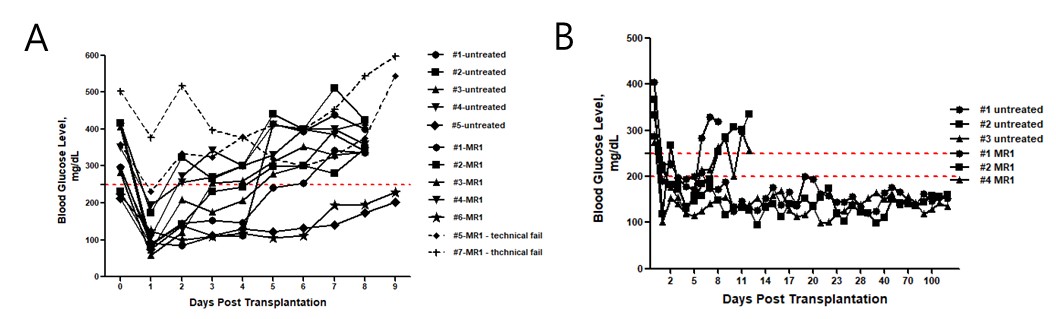
This study was supported by a grant from the Korea Healthcare Technology R&D Project, Ministry for Health & Welfare, Republic of Korea (Project No. HI13C0954) and the National Research Foundation of Korea (Project No. 2016R1D1A1B03930468). .
