Lower Post-Transplant 1 month Tacrolimus Level Less than 10 ng/mL was Associated with Poor Patient Survival in Lung Transplant Patients
JungHwa Ryu1, Tai Yeon Koo1, Sunmi Choi2, Young Tae Kim3, Jaeseok Yang1,4.
1Transplant center, Seoul National University Hospital, Seoul, Korea; 2Department of Pulmonology, Seoul National University Hospital, Seoul, Korea; 3Department of Thoracic Surgery, Seoul National University Hospital, Seoul, Korea; 4Department of Surgery, Seoul National University Hospital, Seoul, Korea
Background: Although lung transplantation has become a standard care for advanced lung diseases, its outcomes are still suboptimal. Low-dose tacrolimus-based immunosuppressant has been considered a standard in kidney and liver transplantation; the optimal therapeutic level of tacrolimus for better survival has not been established in lung transplantation. Therefore, this study aimed to highlight the proper tacrolimus level associated with better outcomes in lung transplant patients.
Method: This retrospective observation study included patients who underwent lung transplantation under tacrolimus-based regimens in the Seoul university hospital between 2006 and 2016. Kaplan-Meier survival analysis and multivariate Cox regression analysis were performed according to tacrolimus trough-levels within 1 year after lung transplantation.
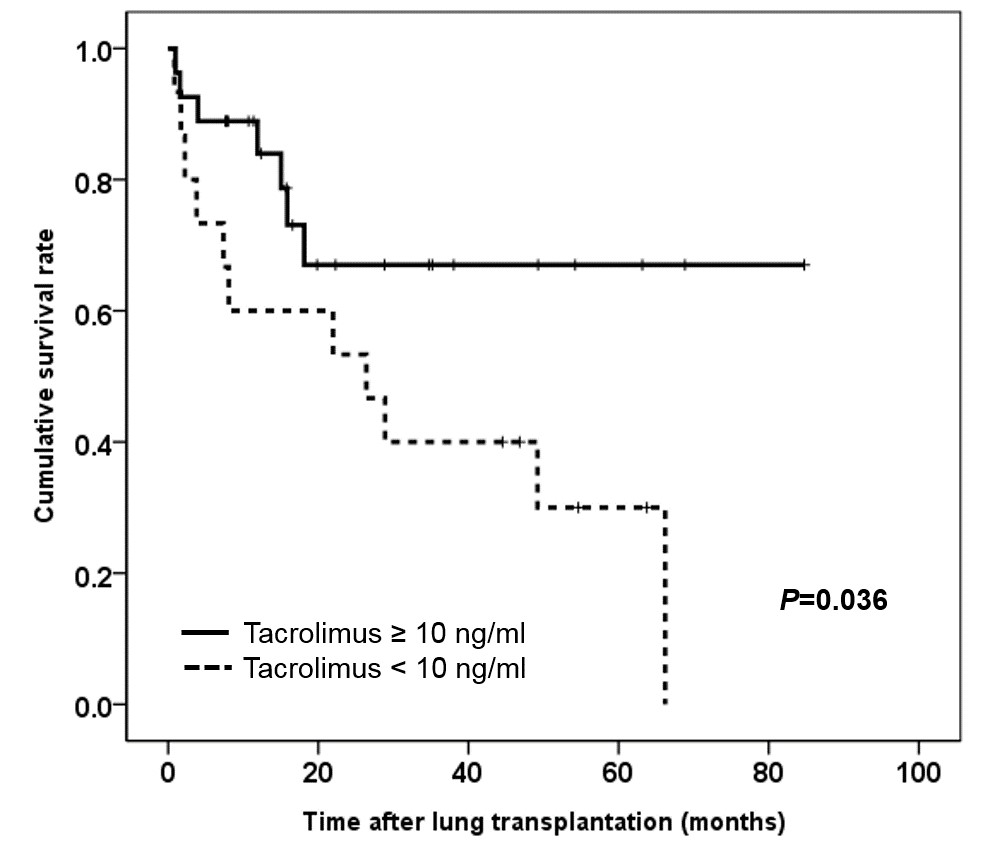
Results: Forty three patients received deceased donor, bilateral lung transplantation and heart-lung transplant patients were excluded. Mean age was 51.1 ± 14.5 years and median follow-up duration was 15.4 months (0-85). The most common transplantation indication was idiopathic pulmonary fibrosis (34.9%). Overall patient survival rate was 55.8% and 1-year patient survival rate was 57.8%. Infection was the most common cause of death (78.9%) and chronic lung allograft dysfunction was observed in 16.3%. The tacrolimus level < 8 ng/mL at 1 month after transplantation was associated with lower rejection-free survival (Log-rank test, P = 0.037). Time-averaged tacrolimus levels < 10 ng/mL within 1 month after transplantation were associated with worse patients survival (Figure, P = 0.036). In multivariate analysis, tacrolimus < 10 ng/mL was also an independent risk factor for poor patient survival (HR 3.506: 95% C.I. 1.143-10.737, P = 0.028).
Conclusion: Keeping sufficient early tacrolimus level (≥ 10 ng/mL) within 1 month after lung transplantation is beneficial for patient survival. More concise monitoring for tacrolimus level might be required at the early phase of lung transplantation.