Safety of Induction Immunosuppression in Kidney Transplantation: Focus on 1-Year Hospitalizations for Infection and Development of Post-Transplant Neoplasia
David Cucchiari1, Alicia Molina-Andujar1, Elena Cuadrado1, Ignacio Revuelta1, Fritz Diekmann1.
1Renal Transplant Unit, Hospital Clínic, Barcelona, Spain
Introduction: it is already known that induction therapy favors the development of infection and post-transplant neoplasia. However, few studies have explored so far the differences between different inductive agents, especially anti-CD25 antibodies and polyclonal anti-lymphocytes antibodies.
Methods: longitudinal analysis of kidney transplant recipients in the Hospital Clínic of Barcelona from 2002 to 2014 (initial n=1753). Recipients of a combined transplant (e.g. kidney-pancreas) or patients with unavailable data were discarded (final n=1448). Patients were divided in three groups according to the administered induction: Group 1) no induction (n=241), Group 2) anti-CD25 antibodies (either basiliximab or daclizumab) (n=593), Group 3) polyclonal anti-lymphocytes antibodies (n=614).
Results: Group 2 patients were older and more likely received a kidney from a living and an older donor. Group 3 had significantly higher percentage of re-transplantation. About maintenance therapy, there was a higher percentage of patients doing mTOR inhibitors in Group 3. Delayed Graft Function was observed more commonly in Group 3 as well. However, no differences were noted in the incidence of rejection and graft failure. Group 3 patients had higher possibility to be hospitalized during the first year of transplantation for an infection compared to Group 2 patients (p=0.025). Number of hospitalizations was increased as well in Group 3 patients compared to Group 1 (p=0.004) and Group 2 (p=0.027), while no significant difference was found between Group 1 and 2 (p=0.161). There was no difference among groups in the development of post-transplant neoplasia (p=0.44). 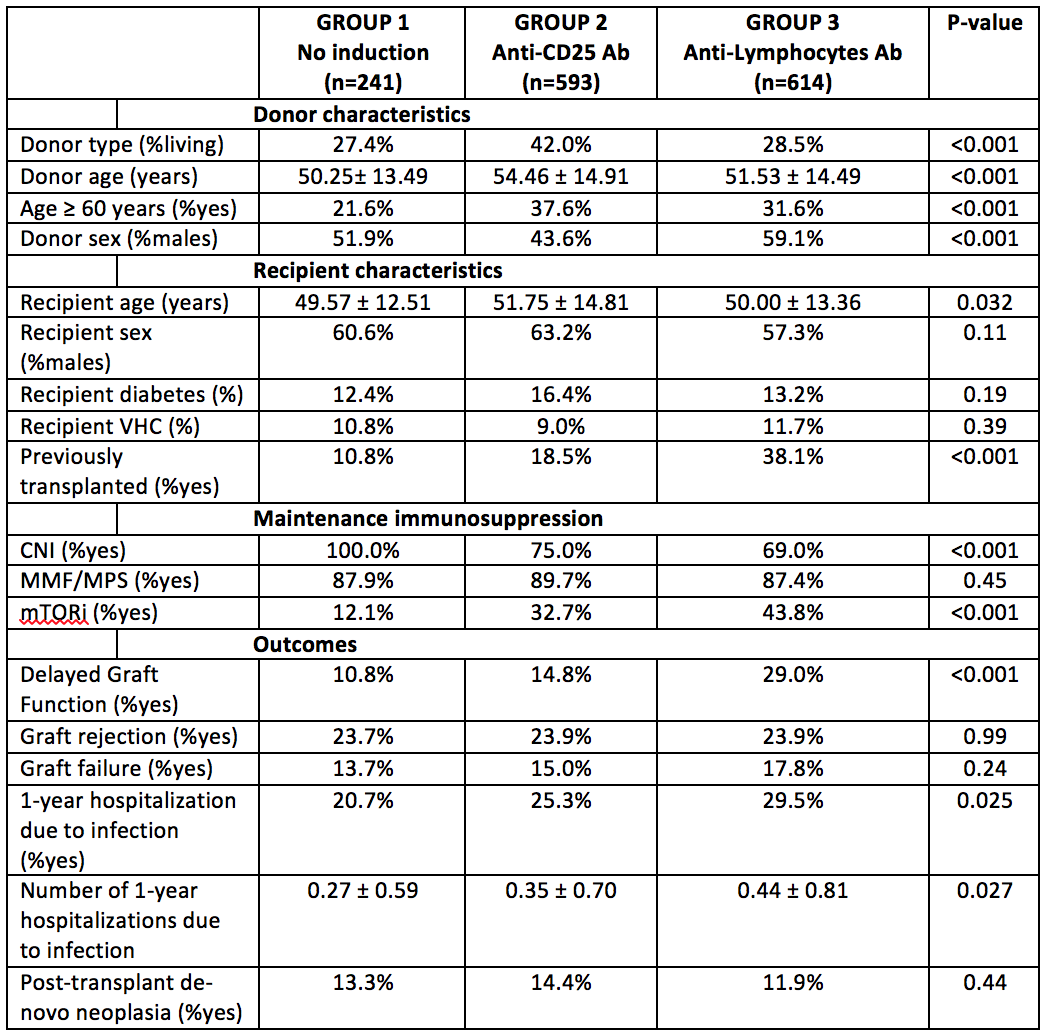
Conclusions: Induction therapy with polyclonal anti-lymphocytes antibodies was associated with a higher likelihood of hospitalization for infection during the first year after kidney transplantation. The number of hospitalizations was increased as well in this group of patients.
