Influence of Immunosuppression on Metabolic Outcomes One Year after Kidney Transplantation: The Role of Mycophenolate and mTOR Inhibitors on Lipid Metabolism and Glycemic Control
David Cucchiari1, Sabine Karam2, Pedro Ventura-Aguiar1, Fritz Diekmann1, Vicens Torregrosa1.
1Renal Transplant Unit, Hospital Clínic, Barcelona, Spain; 2Department of Medicine, Saint George Hospital University Medical Center, Beirut, Lebanon
Introduction: it is widely known that immunosuppressive drugs alter lipids and carbohydrate metabolism in kidney transplant patients. The most common side effects are diabetes mellitus induced by calcineurin inhibitors and hypertriglyceridemia caused by mTOR inhibitors. However, little is known about the combination of these agents in real clinical practice and if a difference exists between patients who were already diabetics or not before transplantation.
Methods: longitudinal retrospective 1-year long study in which we compared two different regimens based on tacrolimus and prednisone, one with mycophenolate (MP group) and one with an mTOR inhibitor (mTORi group). The studied population included all kidney transplanted patients in the Hospital Clínic, Barcelona, performed in a 3-year period from June 2013 to May 2016. Patients who died, lost the transplant or changed the immunosuppression before completion of follow-up were excluded, as well as patients who underwent combined kidney-pancreas transplantation (34.3% of the original population, final n=272). One-year outcomes were changes in total and LDL cholesterol, triglycerides, glycated hemoglobin (HbA1c) and incidence of de-novo diabetes.
Results: considering the global population, patients doing mTORi experienced a more significant increase in HbA1C compared to patients doing MP (mTORi group +0.98 ± 1.13% versus MP group +0.66 ± 1.38%, p= 0.017, for the difference between baseline and 1-year values). There was a substantial increase as well in triglycerides in the mTORi group (MP +1.42 ± 85.83mg/dl versus mTORi +23.21 ± 95.87mg/dl, p= 0.003). 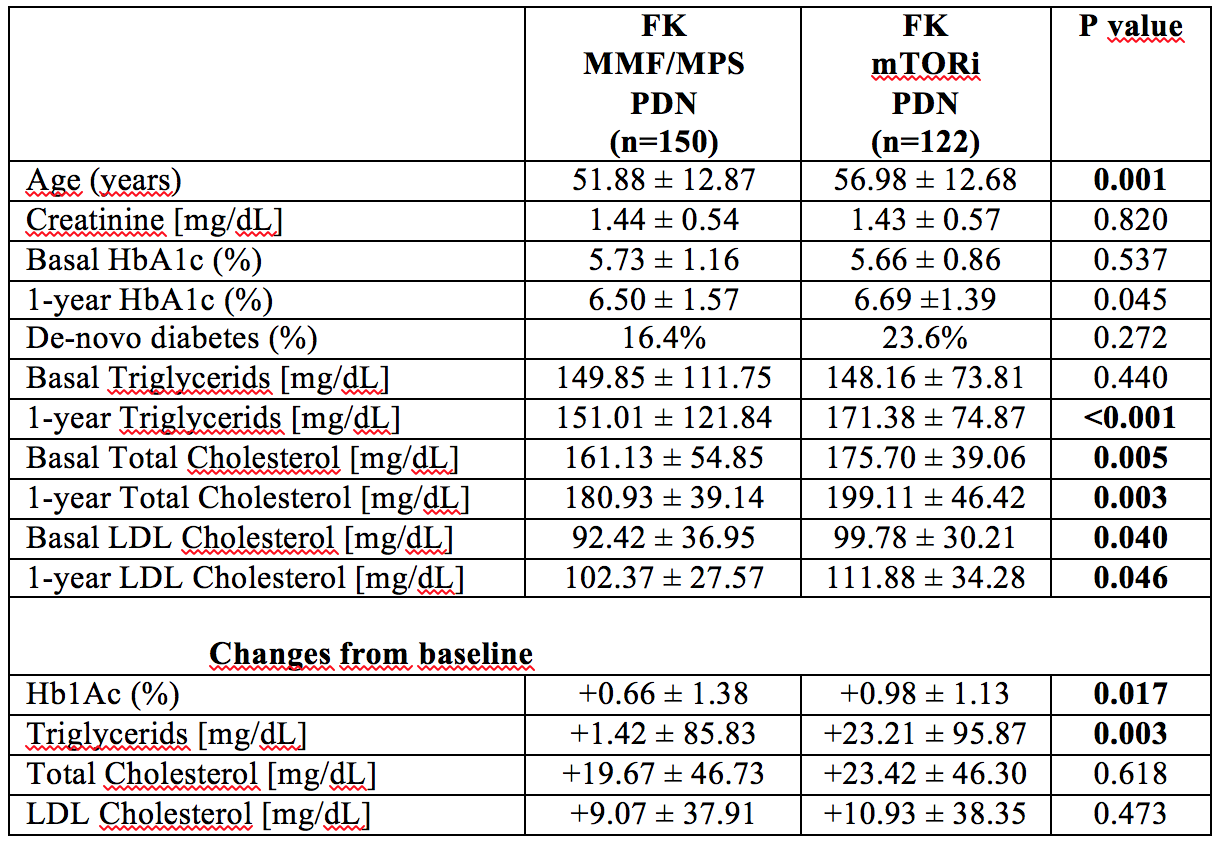 When considering only diabetic patients at baseline (n=73), the increase in HbA1c at 1 year was much more pronounced in patients doing mTORi (MP +0.7 ± 1.97% versus mTORi +1.6 ± 1.31, p=0.020), while there was not substantially any change in triglycerides between the two groups (p=0.879).
When considering only diabetic patients at baseline (n=73), the increase in HbA1c at 1 year was much more pronounced in patients doing mTORi (MP +0.7 ± 1.97% versus mTORi +1.6 ± 1.31, p=0.020), while there was not substantially any change in triglycerides between the two groups (p=0.879). 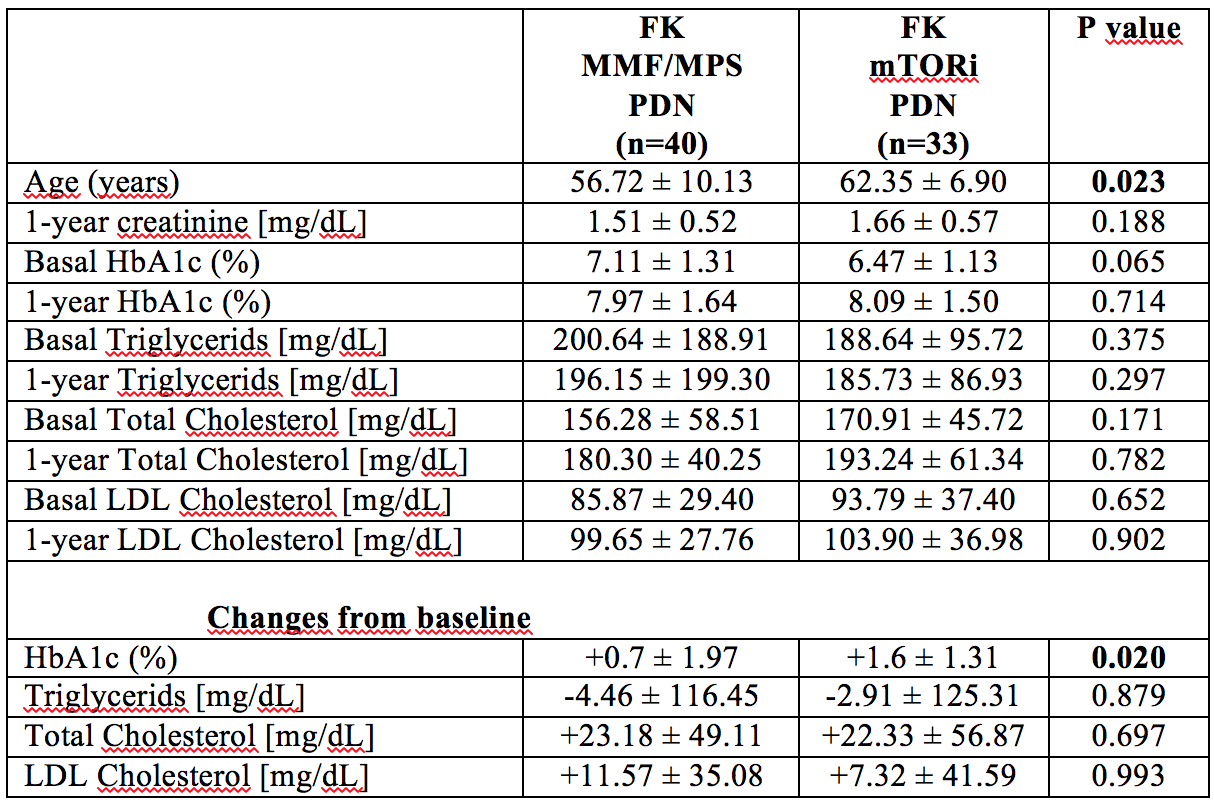 On the contrary, in patients without diabetes at baseline (n=199), the mTORi group experienced a significant increase in triglycerides (MP +1.42 ± 85.83 mg/dl versus mTORi +23.21 ± 95.87 mg/dl, p-value 0.003), while no difference was observed in HbA1c (p-value 0.298). There was no difference in the incidence of de-novo diabetes between groups (p=0.272).
On the contrary, in patients without diabetes at baseline (n=199), the mTORi group experienced a significant increase in triglycerides (MP +1.42 ± 85.83 mg/dl versus mTORi +23.21 ± 95.87 mg/dl, p-value 0.003), while no difference was observed in HbA1c (p-value 0.298). There was no difference in the incidence of de-novo diabetes between groups (p=0.272). 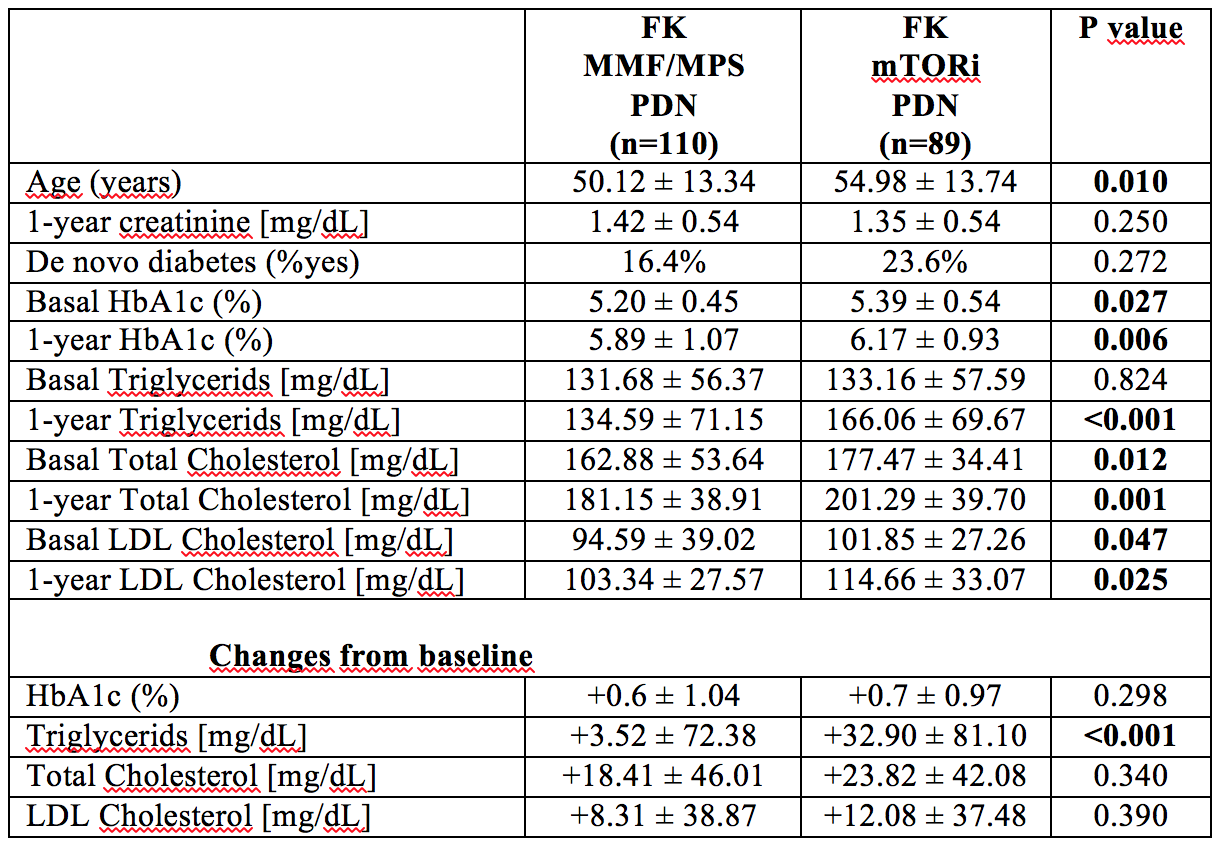
Conclusions: mTOR inhibitors are associated with higher levels of HbA1c and triglycerides 1 year after transplantation compared to mycophenolate, in a tacrolimus- and prednisone-based protocol. However, the change in HbA1c was mainly observed only in mTORi patients who were already diabetics before transplantation and there is not an increase in the incidence of de-novo diabetes. Curiously, the increase in triglycerides was confirmed only in patients who were not diabetics before transplantation. This may suggest that mTOR inhibitors can cause different metabolic abnormalities depending on the original metabolic status of the transplanted patient.
