
Liver Transplantation Outcomes after Acute Liver Failure: Still Some Questions to be Asked
Marina Pérez-Flecha1, Óscar Caso Maestro1, Carlos Miguel Muñoz Arce1, María García-Conde Delgado1, Oana Anisa Nutu1, Leonardo Santiago Salamea Sarmiento1, Alberto Alejandro Marcacuzco Quinto1, Jorge Calvo Pulido1, Iago Justo Alonso1, Carlos Jiménez Romero1.
1General Surgery and Transplantation Department, Haspital Universitario 12 de Octubre, Madrid, Spain
Introduction: Before de use of liver transplantation (LT) in acute liver failure (ALF), mortality of these patients was up to 85%. Today, it is around 20-25%. Despite the good results, ALF has a worse short-term survival compared to other indications. The aim of this study is to evaluate our results in LT after ALF and identify prognostic factors in order to better select patients that will benefit from a LT and save grafts in those cases of unavoidable decease.
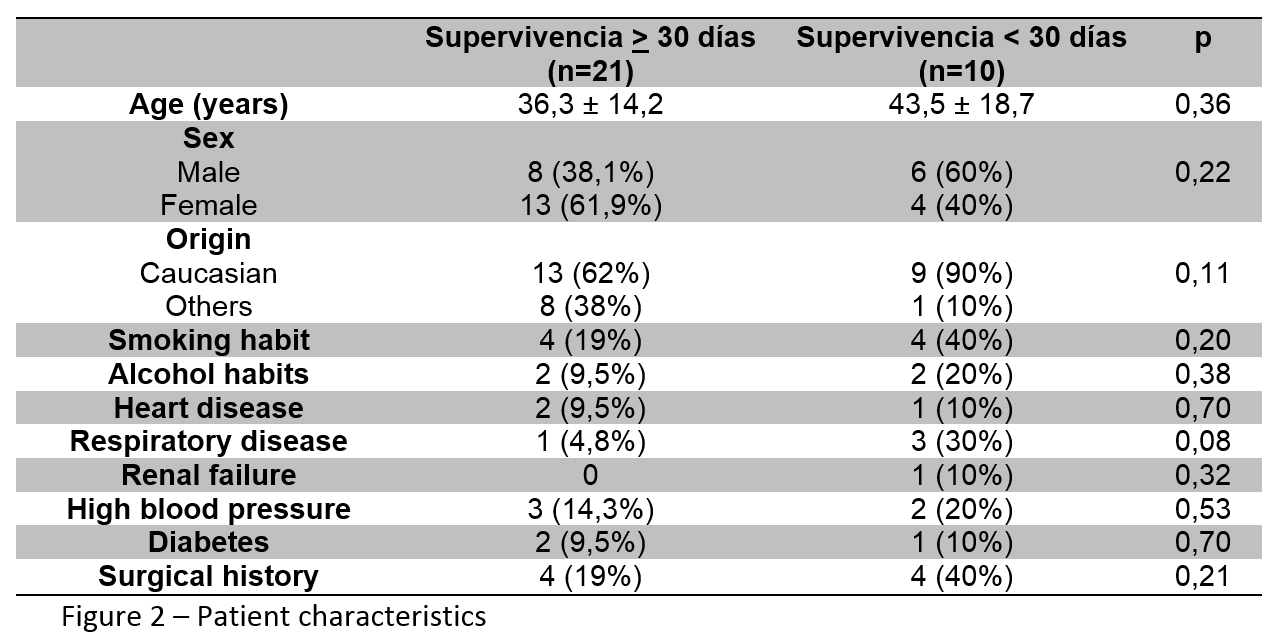
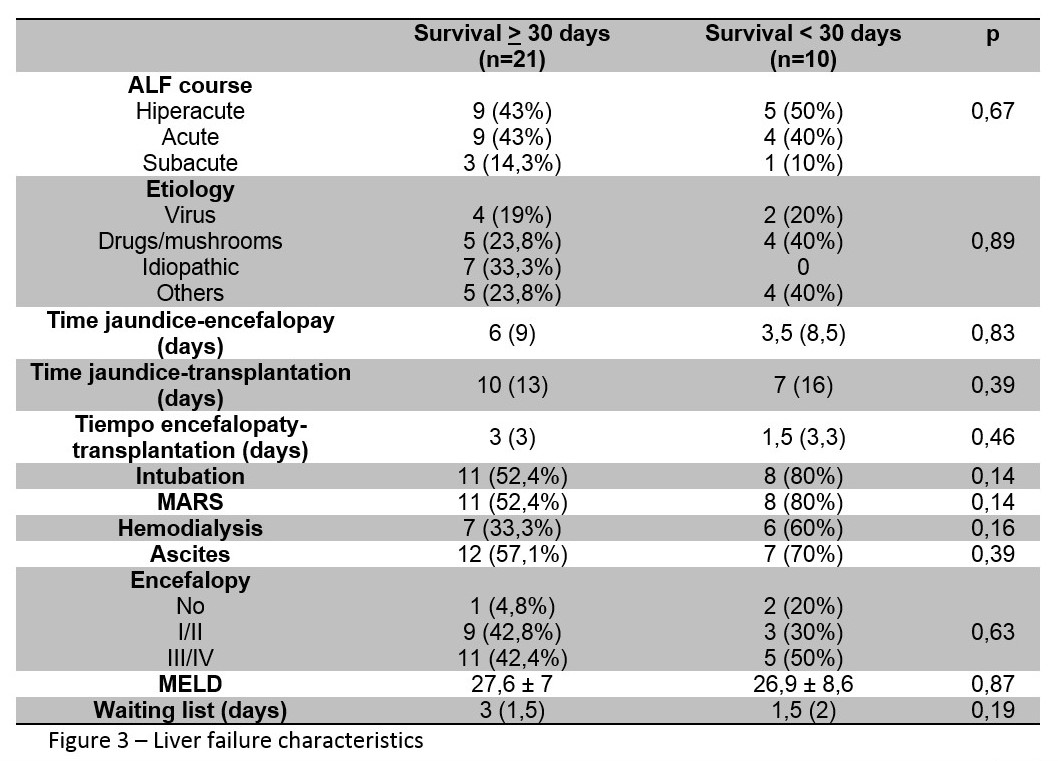
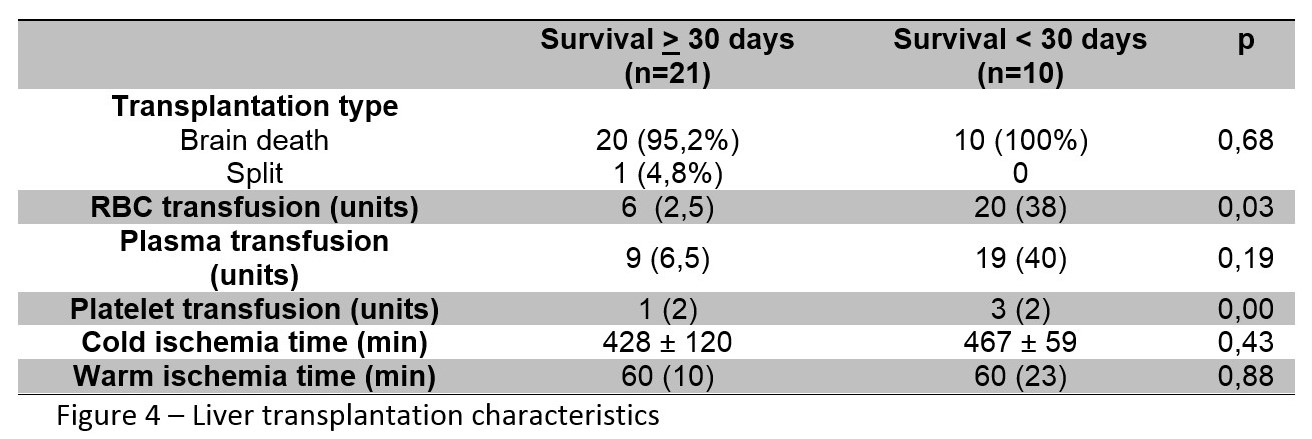
Materials and Methods: We underwent a longitudinal and retrospective study of all patients over 15 years old receiving a LT due to an acute liver failure, from January 2006 to December 2016, in our department. Multiple parameters were evaluated. Patient and graft survival were as well studied. Finally, we compared the characteristics of patients surviving more than 30 days to those deceasing the first month.
Results: During this period we found 31 patients who received a LT to treat an ALF. The mean recipient age was 39 years and 17 (55%) patients were female. We found 8 (25.8%) smokers, 5 (16.1%) patients with hypertension and 8 (25.8%) patients with previous surgical history. The main cause of ALF was drugs (11 patients-35.5%-) followed by virus (6 patients-19.4%-). Hyperacute course was found in 14 (45%) patients. At the moment of the transplantation, 28 (90%) patients had encephalopathy. Orotracheal intubation was required in 19 (61%) patients, vasoactive drugs in 9 (30%) patients and MARS therapy in 19 (61%) patients. Mean MELD score was 27. One of the LT was performed with a partial graft. Median transfusion requirements were in 7 RBC, 10 FFP and 1 PP. Mean cold and warm ischemia time were 426 and 60 minutes, respectively. No cases of primary non-function were present. We identified vascular complications in 1 (3%) patient, biliary complications in 2 (6.5%), infections in 10 (32%) and acute renal failure in 14 (45%). Seven (22.6%) patients developed a rejection. In 2 (6.5%) patients re-transplantation was necessary. Patient and graft survival at 5 years were 75% and 72%, respectively. After the descriptive analysis, we found 21 patients alive after 30 days and 10 patients who died during the first month. We performed a comparative analysis between both groups and we found that previous worse medical status and patients needing intubation or MARS had a poorer outcome. Transfusion requirements were higher in patients surviving less than 30 days, but complication rates were similar between both groups.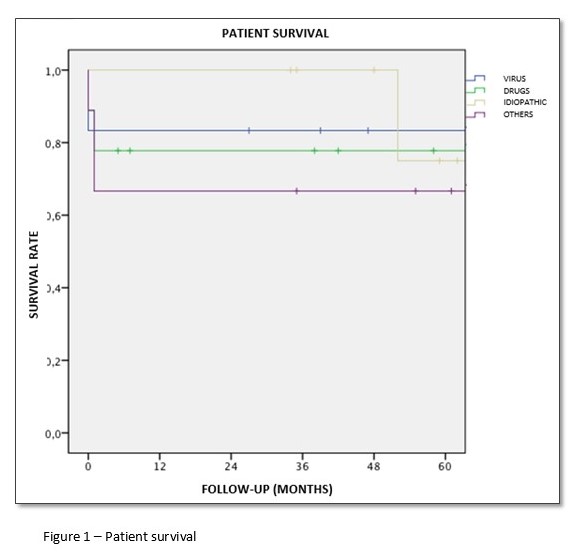
Conclusion: LT is the treatment of choice in ALF not responding to intensive medical treatment. Intubation, MARS therapy, vasoactive drugs and high transfusion requirements were associated with higher mortality rates within 30 days. A longer sample is needed in order to better identify prognostic factors of LT failure after ALF.
