Liver Transplantation as Curative Treatment in Severe Pulmonary Hypertension due to Hepatic Vascular Malformations in Rendu-Osler-Weber Disease
Javier Martínez Caballero1, Jorge J Calvo Pulido2, Alberto Alejandro AA Marcacuzco Quinto2, Lucia L González González1, Iago I Justo Alonso2, Oscar O Caso Maestro2, Pilar P Del Pozo1, Isabel I Montilla Padilla3, Felix F Cambra Molero2, Alejandro A Manrique Municio2, Alvaro A García Sesma2, Luis Carlos C Jiménez Romero2.
1General and Digestive surgery, University Hospital 12 de Octubre, Madrid, Spain; 2Hepato-bilio-pancreatic surgery and transplantation, University Hospital 12 de Octubre, Madrid, Spain; 3Cardiology, University Hospital 12 de Octubre, Madrid, Spain
Introduction: Hereditary haemorragic telangiectasia (HHT) is an autosomal dominant disease characterised by development of arterio-venous malformations (AVM) more common in mucosa, brain, lung, liver and gastrointestinal tract. Pulmonary hypertension (PH) is defined as mean pulmonary arterial pressure (mPAP) > 25 mmHg. Liver transplatation is still controversial in this patients.
Materials and Methods: Woman, 38 years old, with personal history of eclampsia, HELLP síndrome and HHT type 2 (Rendu-Osler-Weber) with exon 9 in the ALK1 gen mutation that presents as systemic manifestations self-limited epistaxis and liver AVM with mainly arterio-systemic intrahepatic shunt which lead to high output cardiac arrest and moderate to severe PH with a NYHA II functional class.
Lung and brain AVM were not observed in radiologic tests and bubble test was positive due to extracardiac shunt (> 6 heart-beats).
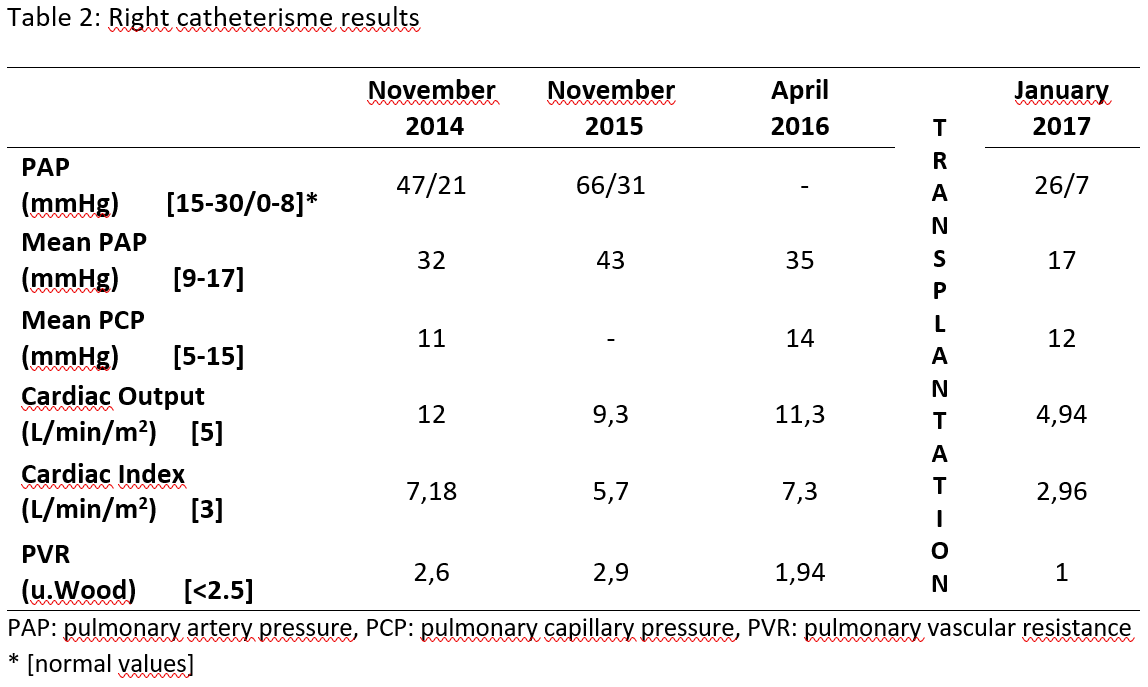
Results: Due to the high risk related to liver transplantation (LT) in this patient, transarterial embolization of liver vascular malformations was performed first, with a 24% reducción in cardiac output (table 1) and development of several complications as intranodal reentry tachycardia and ischemic hepatitis. Because of partial improvement treatment with bevacizumab was iniciated, despite this, the patient suffered recurrent episodes of cardiac arrest and liver function deterioration (MELD 25).
In July 2016, orthotopic LT was performed with a cold ischemia time of 355 min and a warm ischemia time of 40 min, during which he bled profusely requiring massive blood transfusion.
After LT, a 53.2% reduction in the cardiac output was observed in a right catheterism, because extracardiac shunt was eliminated. Furthermore, a pulmonary vascular resistance (PVR) reduction, wich means an absence of vascular branch remodelation, and a normalization in mPAP was shown; which demonstrate the resolution of HP after LT (table 2).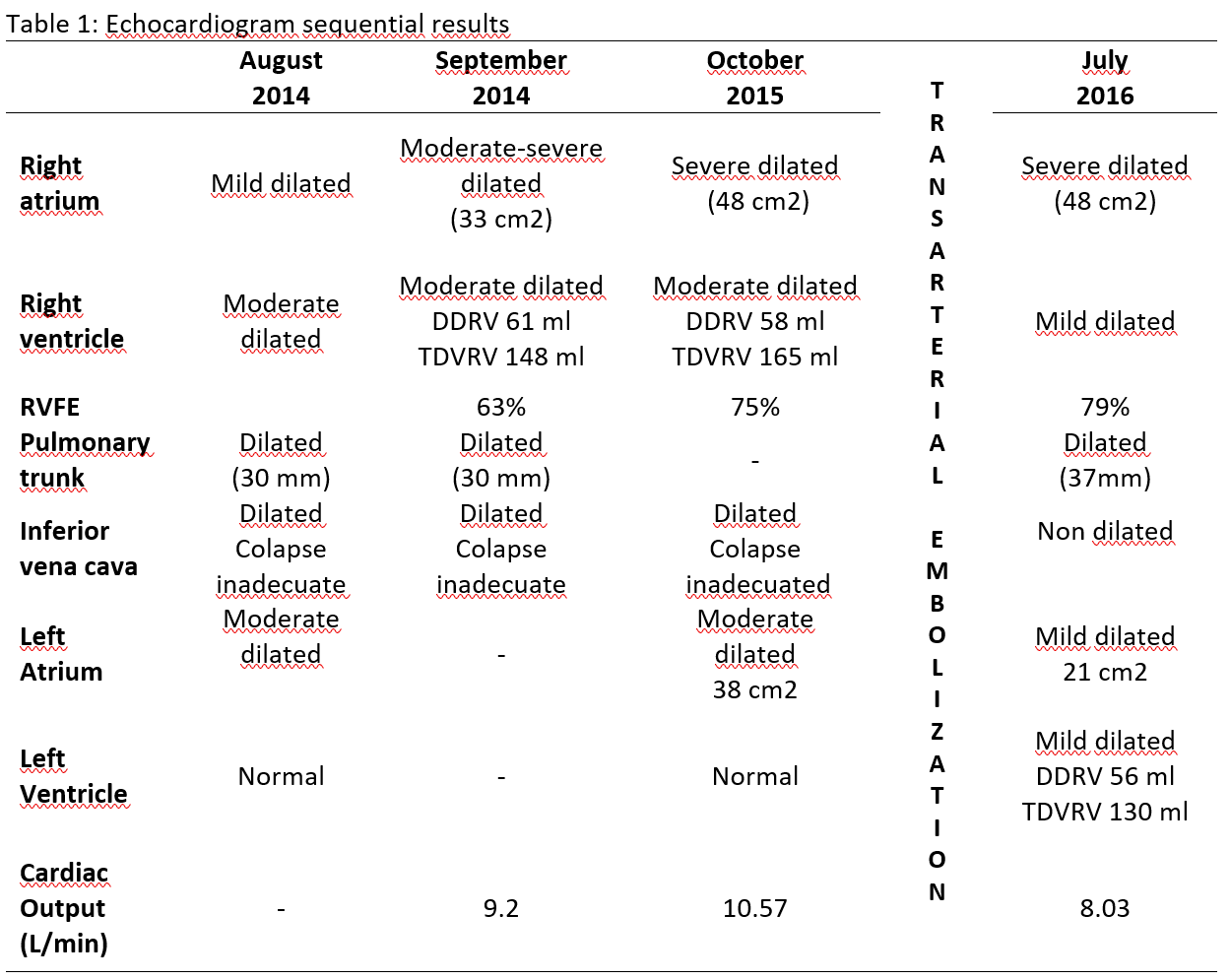
Conclusion:
- LT might be a curative treatment in patients with haemorrhagic vascular diseases if severe HP and cardiac arrest are due to liver AVM
- Liver AVM embolization in moderate-severe HP with elevated cardiac output has mild results
- Diagnosis of Lung AVM causing HP, by angio-TC or angiography, is essential because might contraindicated isolated LT.
