Clinical Significance of Lactate Clearance for the Development of Early Allograft Dysfunction and Short-Term Prognosis in Deceased Donor Liver Transplantation
Deok Gie Kim1, Yoob Bin Jung1, Jee Youn Lee1, Seung Hwan Song2, Jae Geun Lee1, Sung Hoon Kim3, Dai Hoon Han1, Dong Jin Joo1, Man Ki Ju1, Gi Hong Choi1, Jin Sub Choi1, Myoung Soo Kim1, Soon Il Kim1.
1Department of Surgery, Yonsei University College of Medicine, Seoul, Korea; 2Department of Surgery, Ewha Woman’s University College of Medicine, Seoul, Korea; 3Department of Surgery, Yonsei University Wonju hospital, Wonju, Korea
Purpose: This retrospective study evaluated lactate clearance (LC) as a predictor of early allograft dysfunction (EAD) and short-term outcomes in patients receiving deceased donor liver transplantation.
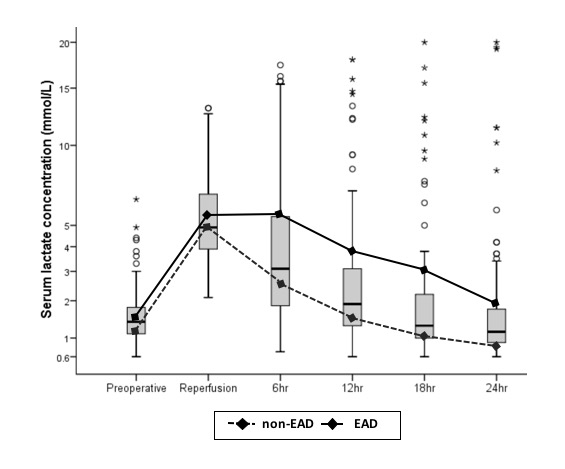
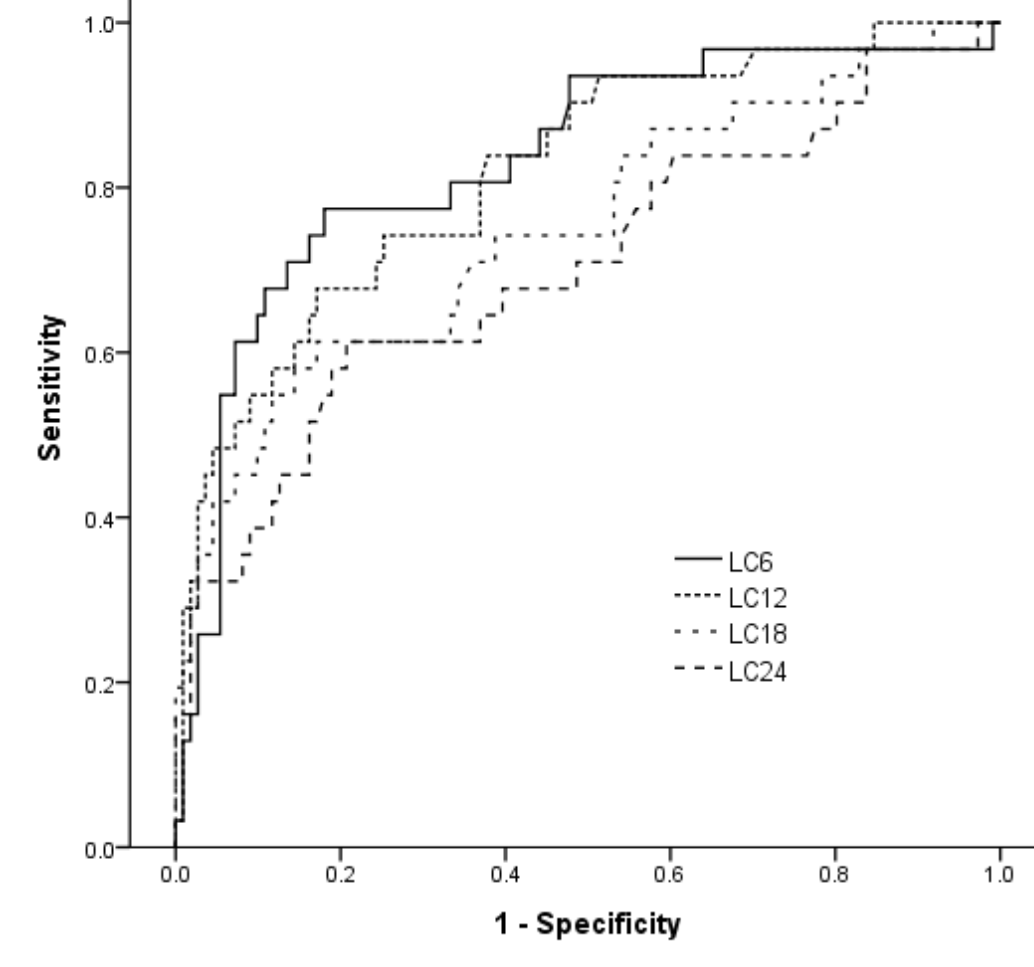
Methods: We performed a retrospective analysis for 181 consecutive deceased donor liver transplantation from January 2011 to May 2016. LCs were calculated at 6, 12, 18 and 24 hours after reperfusion (LC6, LC12, LC18 and LC24).
Results: Of 181 transplant recipients, 44 (24.3%) developed EAD and had lower LCs than those who did not develop EAD. A receiver operating characteristic analysis showed that LC determined at 6 hours showed the highest area under curve value of 0.828 (95% confidence interval [CI]: 0.755–0.990) for predicting the development of EAD at a cutoff value of 25.8% with 76.7% sensitivity and 77.9% specificity. LC values that fell below the cutoff values were significantly associated with EAD in a multivariate analysis, with values at 6 hours having the highest adjusted odds ratio (11.891, 95% CI: 4.469–31.639). In-hospital and 6-month mortalities were higher in patients with LC values below the cutoffs compared with those above the cutoff values at each time point.
Conclusions: LC calculated shortly after reperfusion of an allograft is significantly discriminative for the development of EAD and is associated with short-term prognosis after deceased donor liver transplantation.