
Indications and Timing of Native Nephrectomy for Renal Transplant Recipients with End-Stage Polycystic Kidney Disease. A Literature Review
Christos Nikolaidis1, Argyrou Chrysoula1, Spyridon Vernadakis1.
1Transplantation Unit , Laiko General Hospital, Athens, Athens, Greece
Background: The ideal timing of native nephrectomy in relation to kidney transplantation in patients with autosomal-dominant polycystic kidney disease (ADPKD) can be a very puzzling decision for transplant surgeons and remains a matter of debate. This review article aims to present current literature regarding this highly controversial issue.
Materials and Methods: The MEDLINE/PubMed database was searched using “polycystic kidney disease”, “renal/kidney transplantation” and “native nephrectomy” as key words. Our search was focused on the optimal timing of and indications for native nephrectomy in renal transplant recipients with ADPKD.
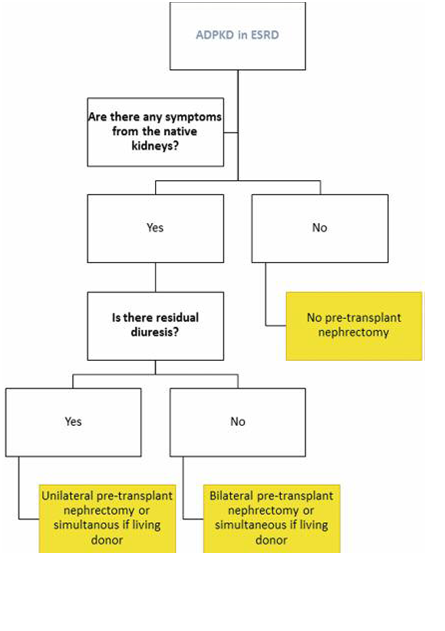
Results: In symptomatic cases, pre-transplant unilateral or bilateral native nephrectomy seems appropriate, in order to alleviate symptoms. In cases that are provided with the option of living-donor transplantation, the performance of the simultaneous procedure could be of benefit. When the principal indication of native nephrectomy is the creation of space for the renal allograft, various studies highlight the safety of the simultaneous approach of either unilateral or bilateral nephrectomy.
Conclusion: No consensus exists on the appropriate timing for native nephrectomy in patients with ADPKD. Several issues to be addressed in the decision-making process are the importance of residual diuresis, the longer operative time along with the associated prolonged ischemia time and higher complication rate of the combined procedure.
