Everolimus Conversion in Kidney Transplant Recipients: Is it Safe?
Seow Yeing Yee1, Mohamad Zaimi Abdul Wahab1, Rosnawati Yahya1, Ravindran Visvanathan1, Ghazali Ahmad1.
1Nephrology, Hospital Kuala Lumpur, Kuala Lumpur, Malaysia
Introduction: The standard immunosuppressive (IS) therapy post kidney transplantation comprised of steroids, calcineurin inhibitor(CNI) and mycophenolate acid. Potential advantages of mammalian target of rapamycin inhibitor(mTORi) include minimization of CNI, improvement of malignancy and cardiovascular risk profile and reduction of cytomegalovirus(CMV) and BK viraemia.
Methods: This retrospective analysis conducted in Hospital Kuala Lumpur reviewed the clinical outcome and adverse events in kidney transplant recipients(KTR) who were converted from standard IS to everolimus(EVR).
Results: 36 KTR were converted to EVR regimen but three received sirolimus prior to EVR. The most frequent combination therapy was EVR, steroids and a CNI.
Majority of KTR were male and half were of Chinese ethnicity. Two thirds(67.6%) of the transplants were from living related donors. 24.3% of KTR was diabetics and 37.8% had hypertension.
32.4% of KTR were converted to EVR after a diagnosis of post transplant malignancy, 18.9% and 16.2% were for CNI minimization and cytopenia respectively. However, the commonest reason for conversion(43.2%) was due to infections with either CMV or BK virus. Five out of 8 patients with CMV infection required concurrent valganciclovir. 8 patients had BK viraemia, including two with BK virus nephropathy. Renal function in both groups of patients remained stable post EVR with undetectable viral load. 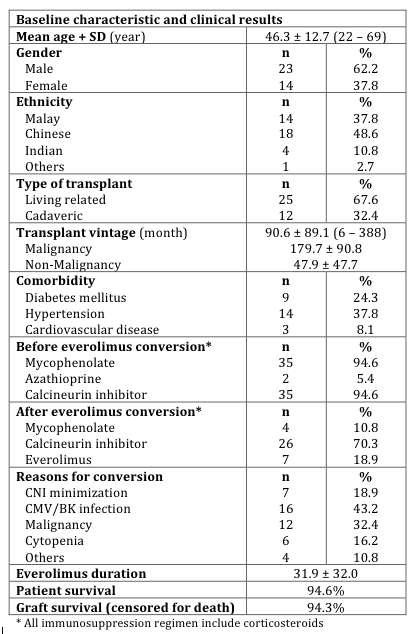
One patient died due to lung cancer and another patient succumbed to necrotizing pneumonia. Two patients had graft failure due to chronic antibody mediated rejection.
There was no increase in acute rejection rate post EVR conversion but there was notable proteinuria development associated with EVR(11.4% versus 37.1%). Seven patients developed oral ulcers(18.9%) and one had oedema but none discontinued EVR. 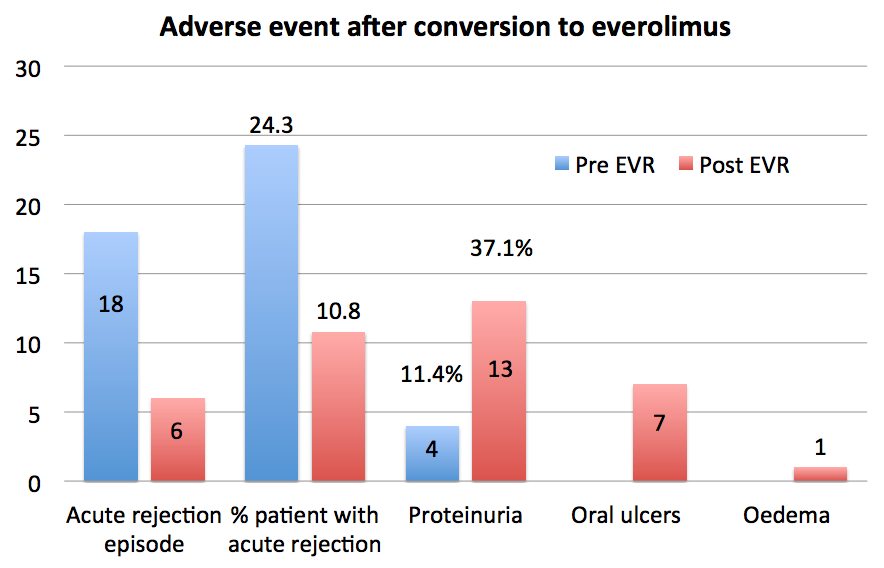
Overall, there was increase in all biochemical values of lipid profile but there was no new cardiovascular event noted. 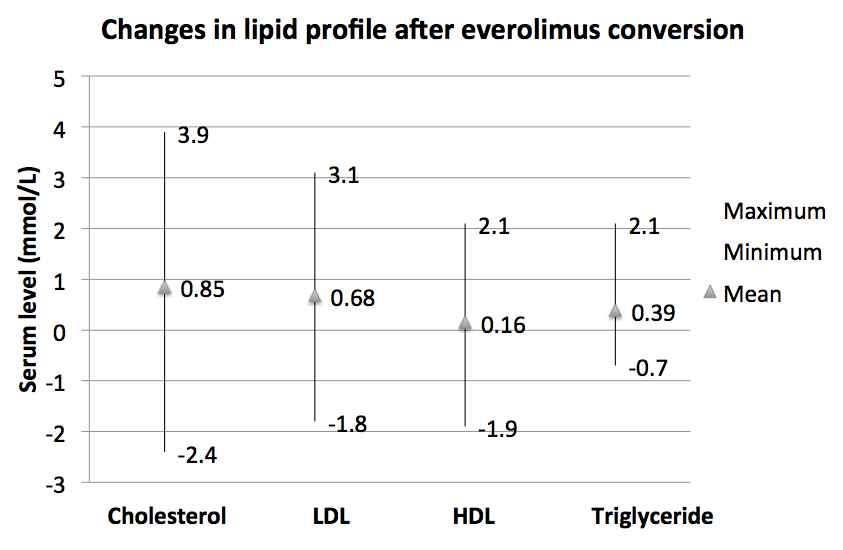 Kidney function remained stable regardless of the baseline estimated glomerular filtration rate(eGFR).
Kidney function remained stable regardless of the baseline estimated glomerular filtration rate(eGFR).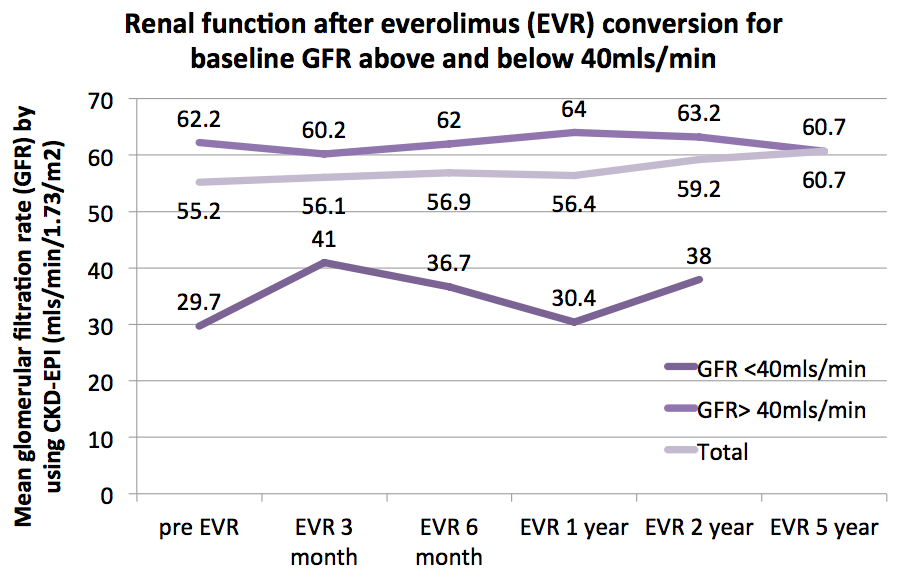
Discussion: Consistent with other reports, our findings showed undectablable CMV or BK viral load post EVR conversion. Due to it’s antineoplastic effect, EVR was increasingly prescribed to improve malignancy risk profile. In our KTR diagnosed with malignancy, there was only one death.
Although there was higher rate of adverse effects compared to other studies, this did not result in discontinuation of the drug. There was no significant improvement of renal function in our cohort with CNI minimization. The major limitations of our study were the small sample size and restrospective, non-randomized study design.
Conclusion: Conversion of standard IS to EVR with either a CNI free or CNI minimization regimen is safe and effective. Renal function and cardiovascular outcome were not adversely affected despite increased proteinuria and worsening of lipid profile.
Adlina Adnan (Transplant Nurse).
