Kidney Transplant in Highly Sensitized Patients: University Malaya Medical Centre’s Experience
Maisarah Jalalonmuhali1, Lim Soo Kun1, Koay Bee Tee2, Lim Soo Jin1, Ng Kok Peng1.
1Division of Nephrology, University Malaya Medical Centre, Kuala Lumpur, Malaysia; 2Institute of Medical Research, Kuala Lumpur, Malaysia
Background: Kidney transplantation is associated with improved survival and better quality of life. In Malaysia, due to limited number of cadaveric as well as compatible Living Related Renal Transplant (LRRT) transplant, there is a need to explore transplant with ABO-incompatible (ABOi) and positive Donor Specific HLA antibodies (DSA). We describe a case series of our experience with kidney transplant in highly sensitized patients.
Objective: The aim of this study is to look at graft function at 1st, 3rd, 6th and 12th months post transplant. Graft functions were assessed by serum creatinine. Apart from that, the likelihood of rejections were notified via protocol biopsy (1st, 3rd, 6th and 12th months post transplant) and DSA level.
Methods: Data was collected from all highly sensitized kidney transplant procedures done in University Malaya Medical Centre (UMMC) between February 2016 and September 2017. Patient’s progress and outcome were documented.
Results: A total of nine patients were recruited during the study period. Table 1 showed the baseline characteristics of the subjects. Immediately post-transplant, patient 1 developed sudden onset of acute hepatitis and patient 2 had sudden onset of shortness of breath. Both patients general conditions only improved after plasma exchange. There were no other obvious causes of their deterioration. We presumed that both patients had acute antibody mediated rejection (ABMR) as a result of preformed DSA.
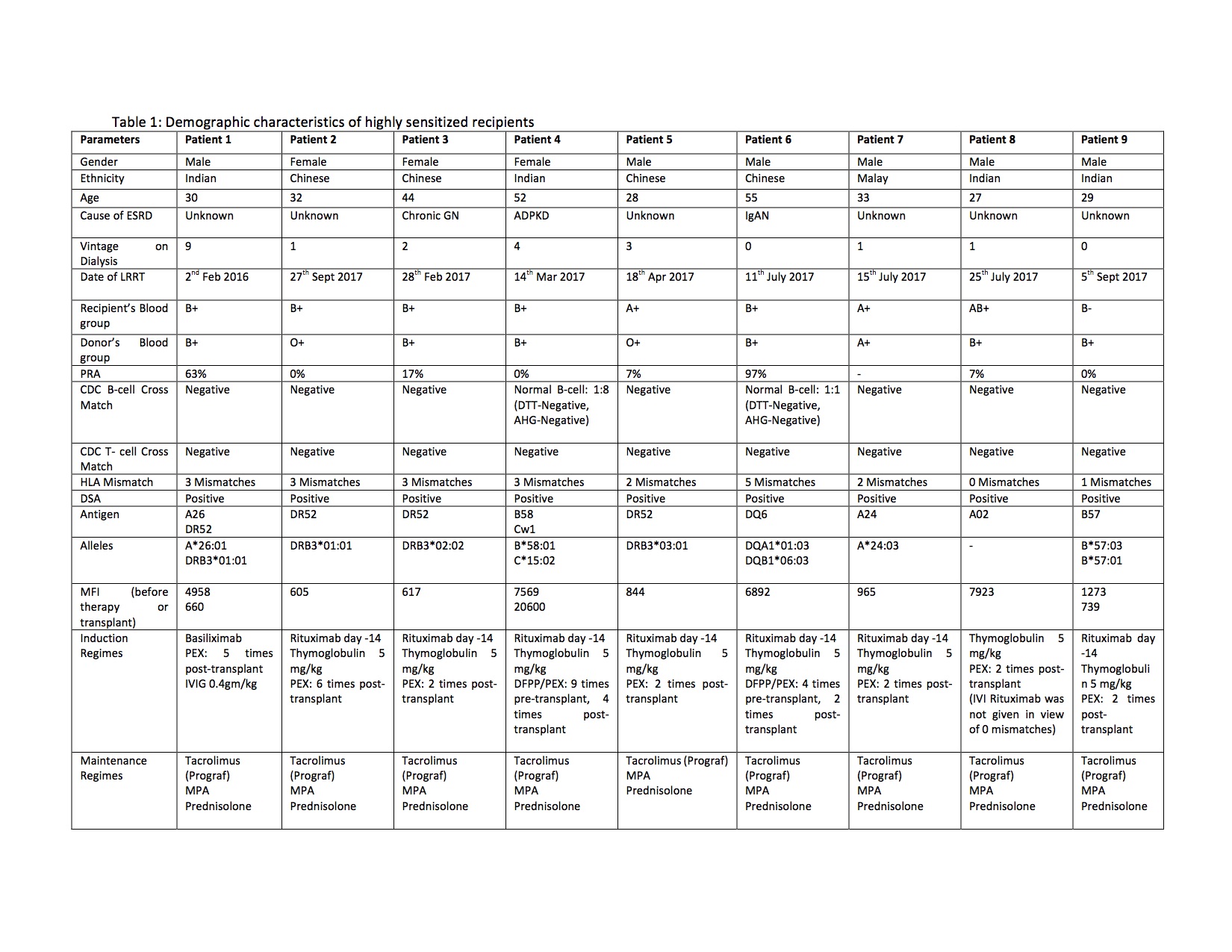
Following our own two experiences we have adopted a protocol consisted of Rituximab at D-14, Methylprednisolone 500 mg at D0, Thymoglobulin D0 until D+4 (total of 5 mg/kg), plasma exchanges for 2 cycles post-transplant (for DSA positive, flow cytometry negative and MFI< 3000). Those patients with MFI > 3000 or positive flow cytometry extra cycles of plasma exchanges needed.
All the patients had achieved immediate graft function. Serum creatinine were stable at 3-month for all the patients, at 6-month for initial 5 patients and at 12 months for the first two patients. Three patients had borderline changes on protocol biopsy but none of them had acute rejection (table 2). At 3 months, DSA level were negative except for patient 1, 4, 6 and 8. For patient 4 and 8 the MFI were reducing in trend. For patient 1 and 6, the MFI were increasing post kidney transplant but protocol biopsy were normal and C4d stained were negative. Their kidney function now stable at 110 and 130 umol/L respectively. None of the patient developed any other de-novo DSA.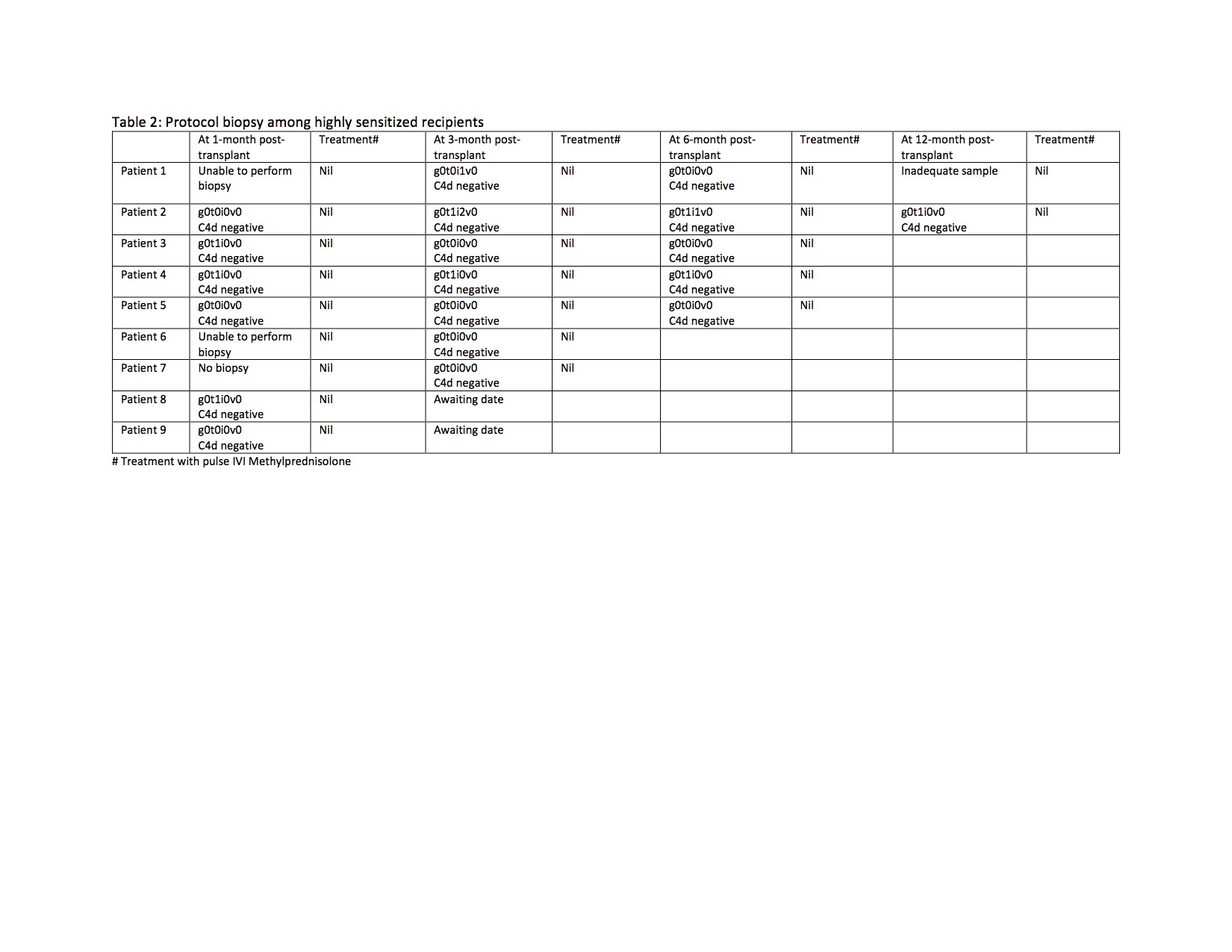 Discussion: Transplant in highly sensitized patient is possible and provided a significant survival benefit. However, early preparation and planning are important. Desensitization protocols may help to overcome incompatibility barriers in live-donor renal transplantation. To date there are various protocol has developed in order to improve short and long term graft survival.
Discussion: Transplant in highly sensitized patient is possible and provided a significant survival benefit. However, early preparation and planning are important. Desensitization protocols may help to overcome incompatibility barriers in live-donor renal transplantation. To date there are various protocol has developed in order to improve short and long term graft survival.
