Importance of Regular Ultrasound Imaging in Renal Allografts for Early Diagnosis of De Novo Renal Cell Carcinoma: A report of Two Rare Cases
Funda Ulu Ozturk1, Nihal Uslu1, Mahir Kirnap2, Mehmet Haberal2.
1Radiology, Baskent University, Ankara, Turkey; 2Transplantation, Baskent University, Ankara, Turkey
Introduction: Renal malignancy development after kidney transplantation (KT) in renal allograft is a rare and an essential long-term complication. Renal cancer occurs mostly in native, end-stage kidneys rather than renal allografts. Prolonged use of immunosuppressive therapy, acquired cystic kidney disease, autosomal dominant polycystic kidney disease are among the increasing factors of malignancy. Renal cell carcinoma (RCC) with a papillary type is the most encountered pathology in allograft kidneys, followed by clear cell type.
Case Reports: We report here two separate cases of de novo clear cell RCC in kidney allografts.
The first case is a 36-year-old female, who was diagnosed end stage renal disease (ESRD) of unknown origin 9 years ago and was performed a living related KT from his father in the following year. Seven years after KT, coming to the clinic with no complaints, on her ultrasonography (US) examination a 2 cm-sized of hyperechoic, hypervascular solid mass was detected in the renal cortex of the allograft (Figure 1).
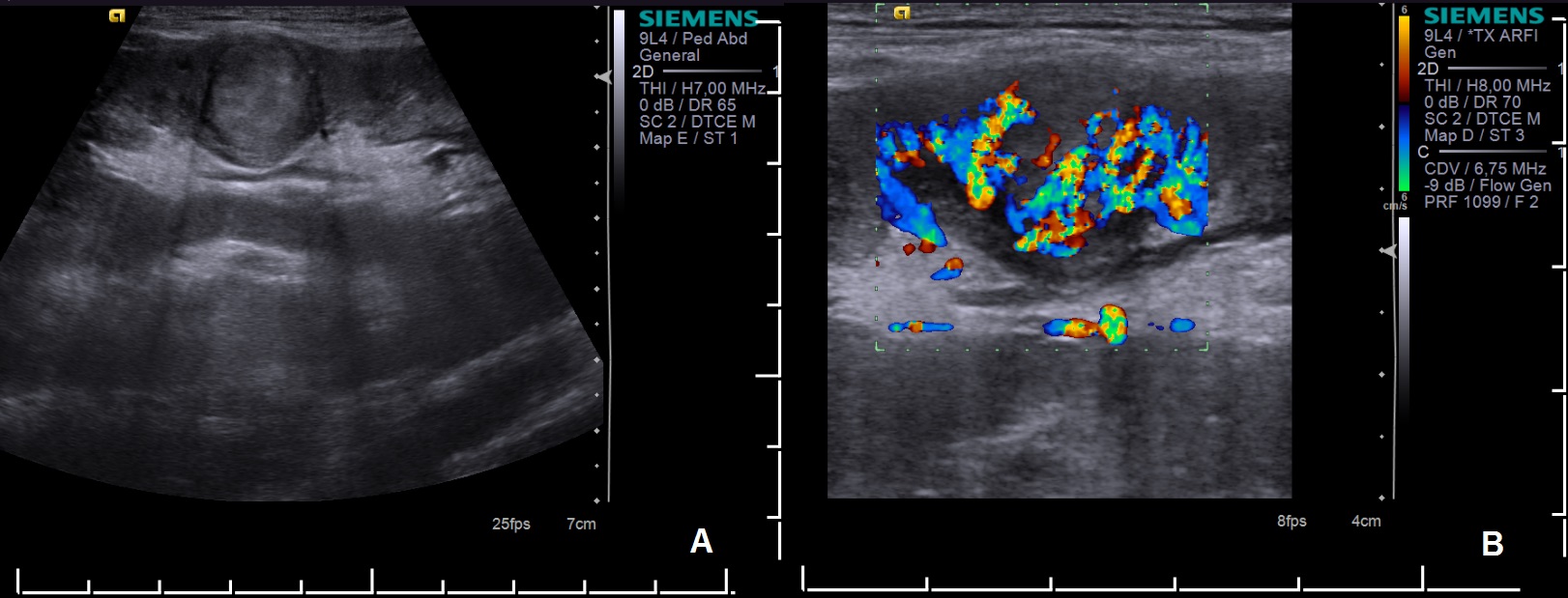
Looking retrospectively to her reports, she was seen to skip her ultrasound follow-ups for the last 2 years. Nephron-sparing surgery was performed after an US-guided stereotactic procedure with a 14-gauge wire. Clear cell RCC of a T1a, N0, M0 tumor with negative margins was reported. The patient is free of recurrence and allograft dysfunction after two years now.
Our second case is a 46-year-old male, who had an ESRD due to pyelonephritis and underwent living related KT from his brother 19 years ago. During annual US follow-ups, a very small hyperechoic nodule was visualised in the posterior cortex of the allograft and short-term US follow-up was suggested. The patient was re-examined in 3 months by a different radiologist and a 9L4 linear transducer was used for screening the graft in addition to the routine 6C1 curvilinear transducer. This revealed multiple foci of hyperechoic nodules in the allograft which could not be determined in the prior US evaluation (Figure 2).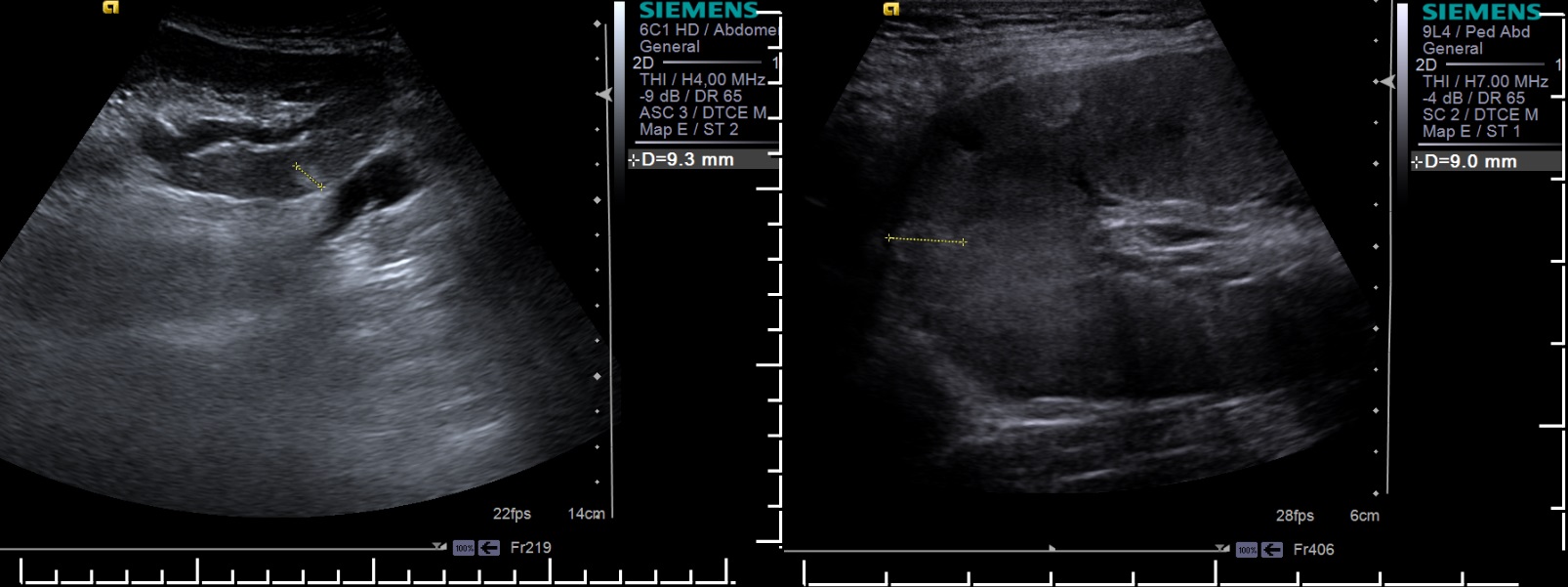
Fine needle aspiration was RCC and no evidence of metastasis was noted with imaging modalities. In order to preserve graft function, nephron-sparing surgery was planned. During surgery, multiple foci were removed, and one in deep location of reach was ablated US-guided with alcohol. After partial nephrectomy, the patient still had millimetric foci of tumors seen on the US, therefore graft nephrectomy was performed in the following months. The patient is in good health now after 1 year, with no evidence of metastasis.
Conclusion: RCC in renal allografts is a rare and increasing malignancy detected after KT. US follow-ups after transplantation regularly with sensitive transducers for a more detailed screening, improves the early diagnosis of this cancer leading to better long-term results and preserving the allograft.
