Prognostic Significance of Microvascular Injury in Kidney Transplant Recipients
Ksenija Vučur1, Mladen Knotek1, Bojana Maksimovic1, Zeljka Jurekovic1, Stela Bulimbasic2, Renata Zunec4, Danica Galesic Ljubanovic3.
1Department of nephrology, University of Zagreb School of Medicine and University Hospital Merkur, Zagreb, Croatia; 2Department of pathology, University of Zagreb School of Medicine and University Hospital Zagreb, Zagreb, Croatia; 3Department of pathology, University of Zagreb School of Medicine and University Hospital Dubrava, Zagreb, Croatia; 4Tissue Typing Center, University Hospital Center Zagreb, Zagreb, Croatia
Introduction: Microvascular injury (MVI), characterized by peritubular capilaritis (ptc) and glomerulitis (g) is one of the histopathological features of AMR, although it can be present in T-cell mediated rejection (TCMR), as well. Preexisting donor specific antibody (DSA) and de novo DSA are associated with the development of acute and chronic AMR, leading to increased risk of graft loss. Recent study showed that MVI score ≥2 was associated with increased intragraft expression of DSA-associated transcripts, higher C4d score, and acute and chronic AMR. However, the prognostic significance of MVI on long-term graft outcome in pts receiving active multimodal rejection treatment has not been studied in detail.
Methods: Retrospective analysis included 63 pts who had kidney transplantation (tx), or simultaneous pancreas and kidney tx (SPKT) at Merkur hospital between 2007 and 2016, with MVI on protocol, or indication bx and available DSA data. Biopsies were scored using the Banff 2015 classification. All pts received treatment for graft rejection and in 94% of pts follow-up bx after treatment was performed.
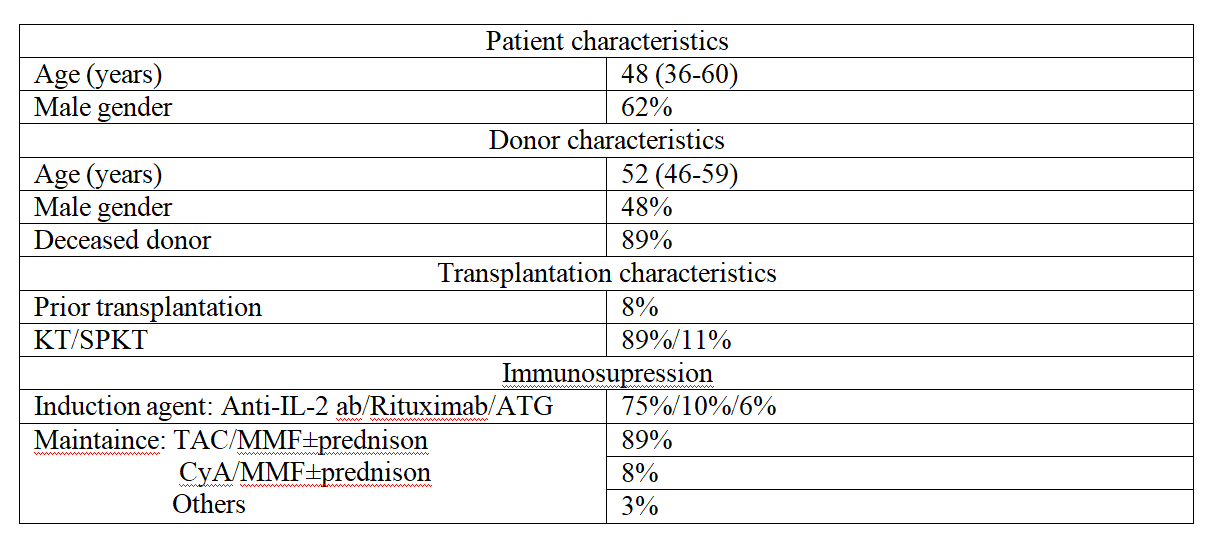
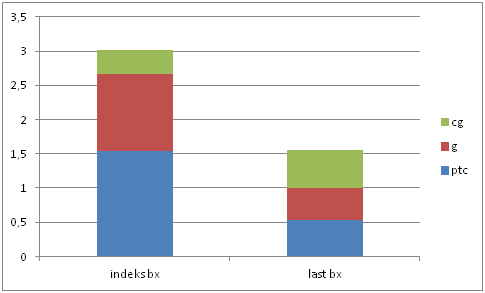
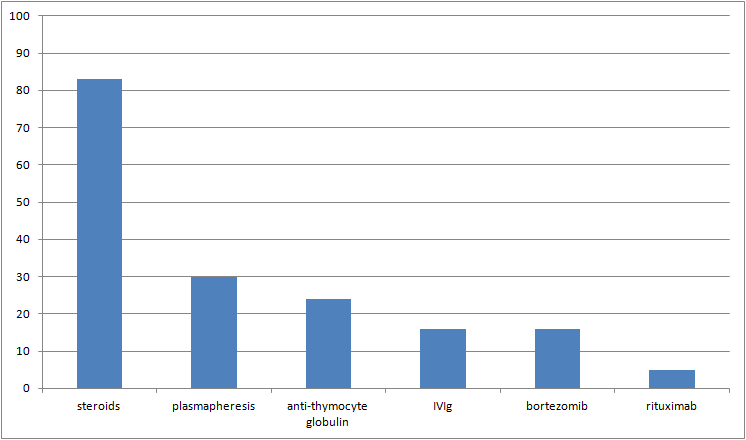
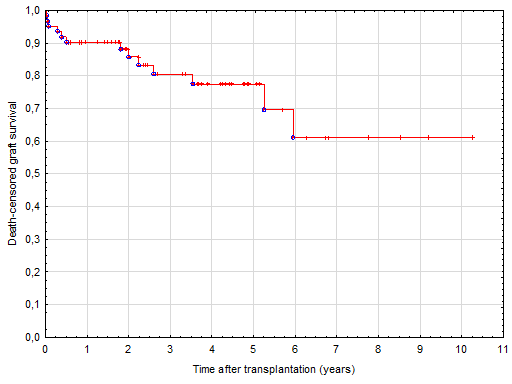
Results: The baseline pt characteristics are shown in Table 1. The median time post-transplant at detection of MVI was 18 days (IQR 9-181). 68% of pts experienced early graft rejection (within 90 days from tx). Glomerular filtration rate at the time of index bx was 26±18 ml/min/1.73m2. 41% of pts had preexisting, or de novo DSA. Among pts with de novo DSA, class I was present in 11%, class II DSA in 29%, and both class I and II in 8% of pts. The average bx number per was 3.2±1.5. At index bx the mean ptc+g score was 2.7±1.4, and 16% had transplant glomerulopathy (cg), whereas on the last bx the mean ptc+g score was 1.0±1.5 (p=0.46), and 18% had cg (p<0.001) (Figure 1). Cumulative rejection treatment included steroids (83%), plasmapheresis (30%), anti-thymocyte globulin (24%), IVIg (16%), bortezomib (16%), and rituximab (5%) (Figure 2). During the median follow up period of 2.4 years (IQR 2-5) death-censored graft survival (DCGS) was 62% (Figure 3). In univariate analysis that included demographic, patohistological, and immunological variables, rituximab treatment was associated with low risk for death censored graft loss (DCGL) (HR 0.1, 95% CI 0.02-0.5, p=0.008), whereas on the last bx after treatment C4d staining (HR 2.05, 95% CI 1.2-3.4, p=0.005), t score (HR 2.69, 95% CI 1.3-5.5, p=0.007), and i score (HR 2.54, 95% CI 1.4-4.6, p=0.002) were associated with DCGL. In multivariate analysis no single variable on index bx was independently associated with DCGL, while on the last bx only C4d staining remained independently associated with DCGL (HR 1.75, 95% CI 1.02-2.9, p=0.04).
Conclusion: Our results show that MVI and DSA may not be independently associated with DCGL in pts receiving active multimodal rejection treatment. Persistent peritubular capillary C4d staining remained independently associated with DCGL.