
Perioperative Hemoglobin and Delayed Graft Function in Kidney Transplant Recipients
Sarah MacIsaac1, Agnihotram Ramankumar1, Nasim Saberi2, Veronique Naessens1, Marcelo Cantarovich1, Dana Baran1, Steven Paraskevas2, Jean Tchervenkov2, Prosanto Chaudhury2, CheeLoong Saw1,2, Shaifali Sandal1.
1Medicine, McGill University Health Center, Montreal, QC, Canada; 2Surgery, McGill University Health Center, Montreal, QC, Canada
Background: A Cochrane review of 31 trials reported no mortality or morbidity advantage with a liberal over restrictive transfusion strategy. Most centers use an absolute hemoglobin concentration (Hb) threshold of 70 g/L for transfusion, unless patients have active cardiac ischemia. However, recent studies have suggested that relative change in hemoglobin levels (∆Hb) is more predictive of patient outcomes. No such analysis has been done in patients undergoing a kidney transplantation, where procured grafts are at high risk of acute tubular necrosis due to ischemia. Given this, we aimed to analyze the relationship between delayed graft function (DGF), and Hb and ∆Hb during transplant.
Methods: We conducted a single-center retrospective chart review of all adult, deceased donor kidney transplants between 2003 and 2017. Recipients of simultaneous multi-organ transplants and those that received a transfusion within the first 24 hours were excluded. Hb was captured at various time points within the first 24 hours post-transplant. ∆Hb was defined as = [(pre-transplant Hb – nadir post-transplant Hb)/pre-transplant Hb] x 100. The outcome of interest was DGF, defined as the need for dialysis within the first week post-transplant. We excluded transplants that had primary non-function.
Results: Of the 934 transplants, 705 were eligible for analysis. Of these 25% (176) experienced DGF. Several baseline differences were noted in those that experienced DGF. Amongst those recipients that developed DGF, Hb values pre-transplant, the lowest Hb post-transplant or ∆Hb were not statistically different from those that did not develop DGF (Table 1). In a univariate analysis, only pre-transplant Hb but not the lowest Hb post-transplant or ∆Hb were predictive of DGF (Table 2). This effect lost significance in a multivariate analysis." href="http://confman.tts2018.org/papers/body/2485#">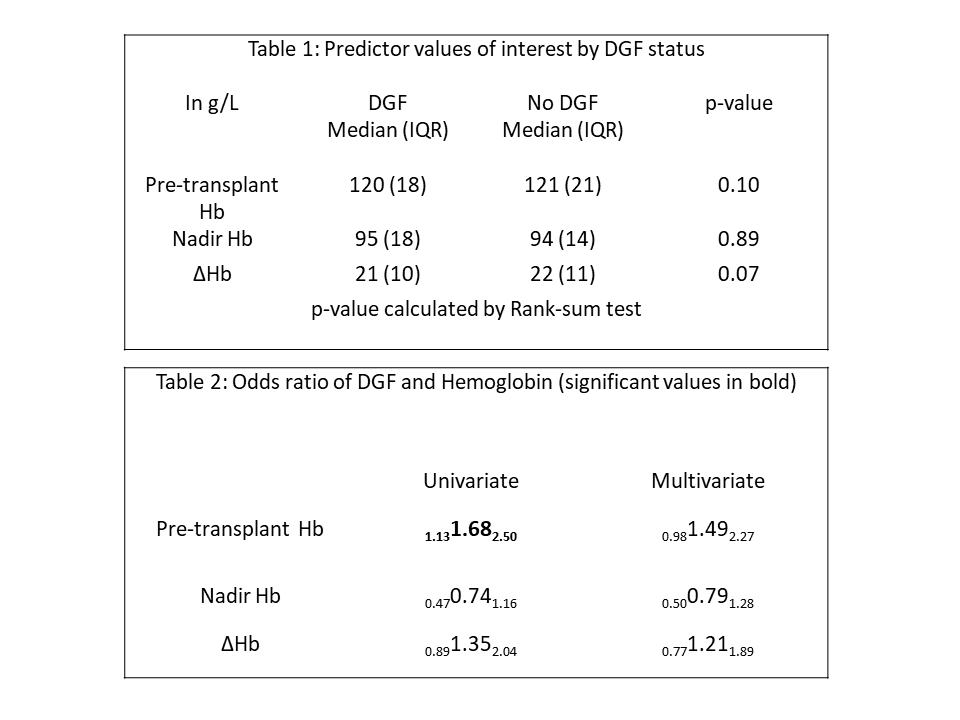
Conclusion: In those recipients that did not receive a blood transfusion perioperatively, the relative change in hemoglobin post-transplant was not predictive of DGF. Future work entails analyzing outcomes in those that received a transfusion. Given the risk of sensitization with blood transfusions, our work supports current restrictive transfusion practices in the kidney transplant population.
