
Panel Reactive Antibody Positivity and Associated Human Leukocyte Antigen Antibodies in Filipino Kidney Transplant Candidates at the National Kidney and Transplant Institute
Bryan Christian Ilagan1, Concesa B. Cabanayan-Casasola1, Florecita R. Padua2.
1Adult Nephrology, National Kidney and Transplant Institute, Quezon City, Philippines; 2Laboratory Medicine, National Kidney and Transplant Institute, Quezon City, Philippines
Introduction: Kidney transplantation is the treatment of choice for patients who have end stage renal disease (ESRD). Factors like panel reactive antibody (PRA) sensitization is one of the most important barriers precluding KT due to increased risk of graft failure.This study determined the PRA status and patient outcome among KT candidates at NKTI.
Materials and Methods: Transplant candidates aged > 18 years who underwent initial PRA determinations in NKTI from July 1, 2013 to June 30, 2016. Frequencies and percentages of demographics and anti-HLA antibodies were calculated. Chi-square and Fisher exact tests were used to compare percentages between groups. 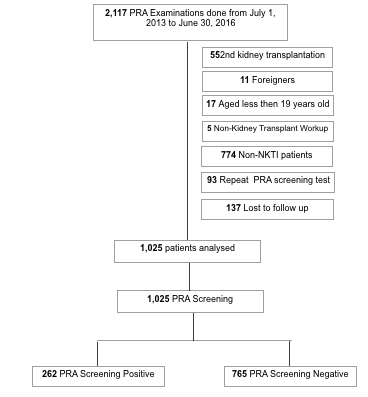
Results: The incidence of sensitized patients is 25.6% with 1:1 male:female ratio. Factors that were statistically significant in the PRA positive compared with PRA negative group: female gender, blood transfusion (BT) history and history of pregnancy. There was a difference in the rate of KT in both groups but not statistically significant. Out of 262 PRA screening positive KT candidates, 11.8% had DSA. Among those with (+) DSA, 42% patients had KT and 58% had no KT. For those patients who did not have KT, 6% died . Among the 262 sensitized KT candidates, 71% had KT. Most of which had KT during the 12-24th month from the time of initial PRA sensitization. For the 29% who did not have KT, 2% died and 27% remained on dialysis. 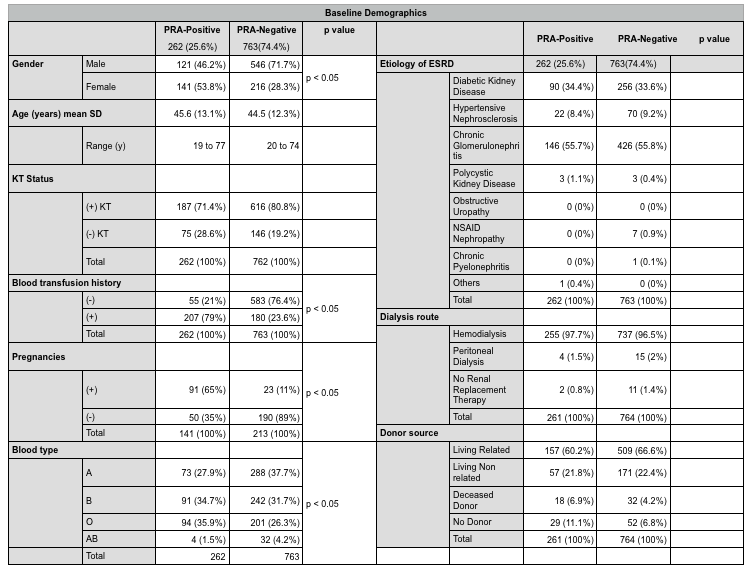
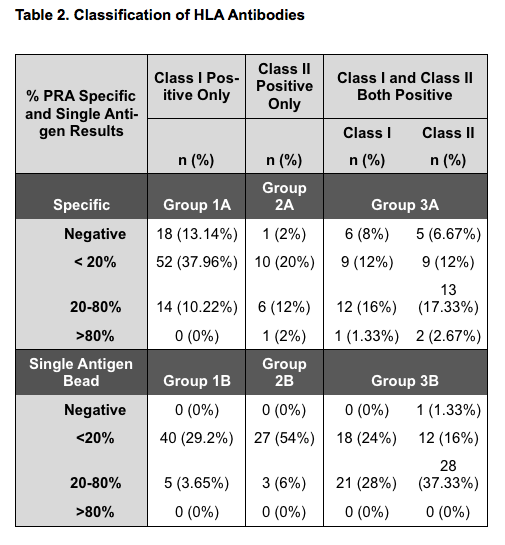
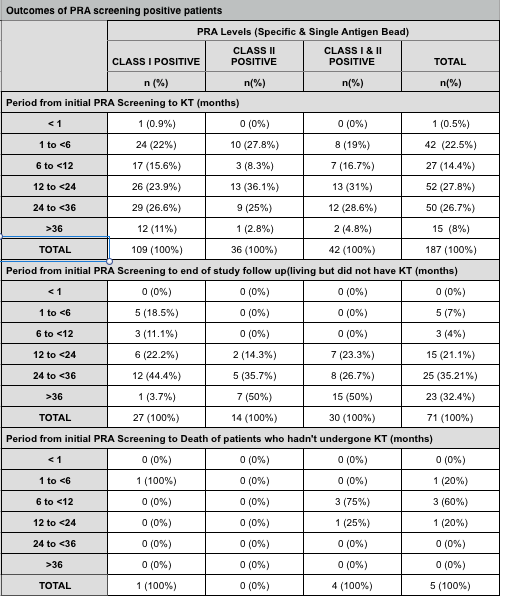
Discussion:The incidence of PRA sensitization is similar to the French (25%) and American (32%) studies. For class I, B antibodies account for the majority of cases in PRA Specific and A and B antibodies for PRA Single Antigen Bead (SAB). While for Class II, high incidence of DR occurrences can be noted in both PRA specific and PRA SAB. These values correspond to the most common HLA antibodies found in the Turkish study but differ in the HLA-specific antibodies which may be due to racial variation and difference in exposure to sensitizing events. In our study most patients had KT during the 365-730 days from the time of initial PRA sensitization in contrast to US data where patients with < 30% PRA had KT after 493 days versus patients with ≥ 30% PRA who waited for 1047 days.
Conclusions: The incidence of sensitized patients is 25.6% which is comparable to Western studies. Female gender, blood transfusion history and history of pregnancy were factors noted to be associated with PRA sensitization. Sensitizing events particularly BT, should be avoided. Paired-exchange program can be considered to hasten KT rate and decrease waiting time for KT. Such program is not yet implemented here in the Philippines. Ethical and possible legal concerns could be of challenge but this could be considered for sensitized patients.
