Is it Really Necessary to Remove anti-A/B Antibodies in ABO-Incompatible Kidney Transplantation?
Yuki Nakagawa1,2, Kazuhide Saito1, Masayuki Tasaki1, Kota Takahashi1, Yoshihiko Tomita1.
1 Department of Regenerative and Transplant Medicine, Niigata University, Niigata, Japan; 2Department of Urology, Uonuma Institute of Community Medicine Niigata University, Niigata, Japan
Introduction: It is well known that blood type antigens cause humoral rejection in ABO-incompatible living-related kidney transplantation (ABO-ILKT) because of preformed natural antibodies directed against the donor blood group. To remove anti-A/B antibodies, the recipients receive 2 or 4 DFPP or PEX sessions before the transplantation until the anti-A/B antibody titers have decreased to ≦1:32. We compared recipients who had induction period immunosuppressive therapy with and without removing of anti-A/B antibodies
Methods: Forty-nine ABO-incompatible renal transplant recipients were enrolled in our prospective study. ABO-I-NRA Group (ABO-I without removing anti-A/B antibodies)(n=30) patients received desensitization without methods of removing anti-A/B antibodies during January, 2010 - July, 2017 ABO-I-RA Group (ABO-I with removing anti-A/B antibodies)(n=19) was a control group. We also studied 19 ABO-ILKTx patients with DFPP/PEX/ Immune adsorption during February, 2009 - July, 2017.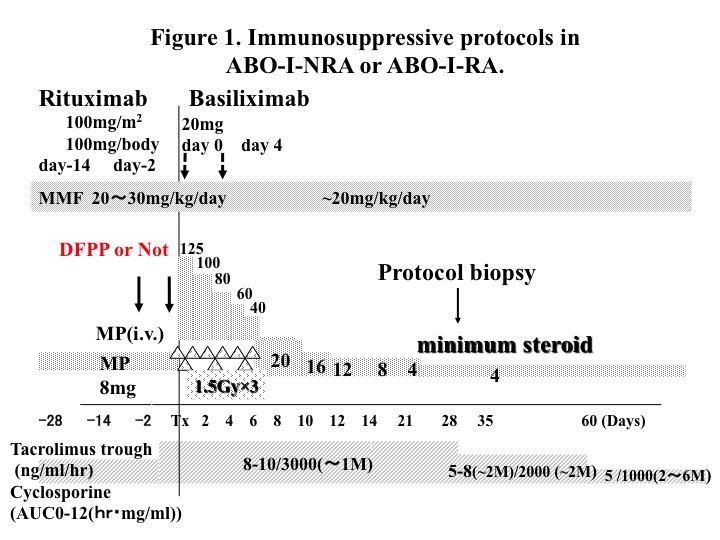
Results: 1. Patient (100%versus 100%) and graft and survival (100% versus 95%) at 1 year were no different between the groups. 2. Patients of ABO-I-NRA Group experienced less acute rejections than those in ABO-I-RA Group (7.1% versus 38.8%, P=0.053), the difference not significant.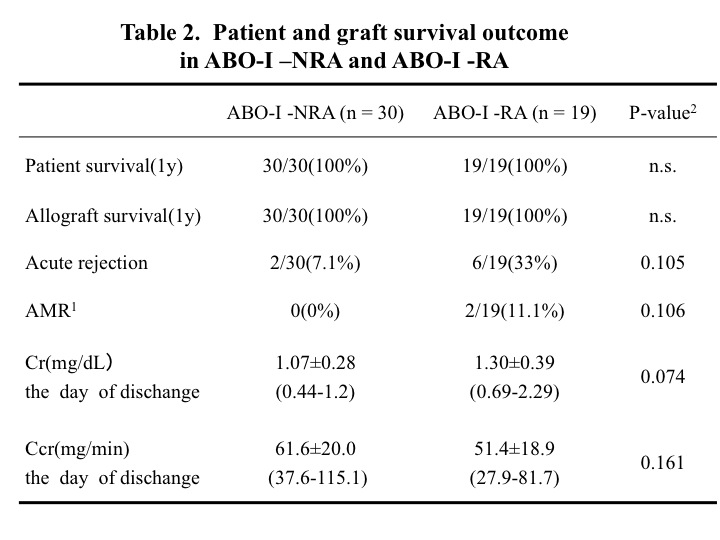 3. Two patients (2/19: 10%) in the RA group developed antibody-mediated rejection (AMR). One patients (1/19: 5.2%) in the RA group who developed thrombotic microangiopathy(TMA) was graft loss. There were no significant differences between the two groups with regards to other adverse events. 4. There were no significant differences in the rates of change in anti-A/B antibody (IgG), anti-A antibody (IgM/IgG),or anti B-antibody (IgG) between 1 month pretransplant and at the time of transplant, or between 1 month pretransplant and 1 month posttransplant.
3. Two patients (2/19: 10%) in the RA group developed antibody-mediated rejection (AMR). One patients (1/19: 5.2%) in the RA group who developed thrombotic microangiopathy(TMA) was graft loss. There were no significant differences between the two groups with regards to other adverse events. 4. There were no significant differences in the rates of change in anti-A/B antibody (IgG), anti-A antibody (IgM/IgG),or anti B-antibody (IgG) between 1 month pretransplant and at the time of transplant, or between 1 month pretransplant and 1 month posttransplant.
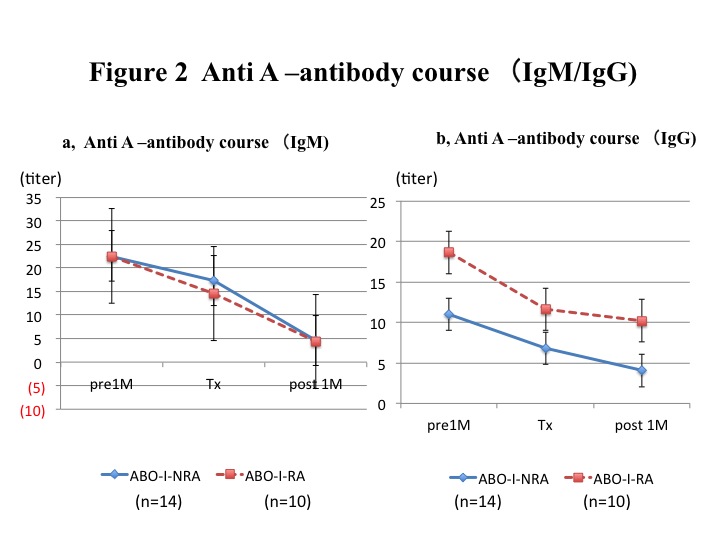
5. On the other hand, a significantly higher rate of change (reduction rate) was seen in the RA group than in the NRA group with regards to anti-A/B antibody (IgM) and anti B-antibody (IgM).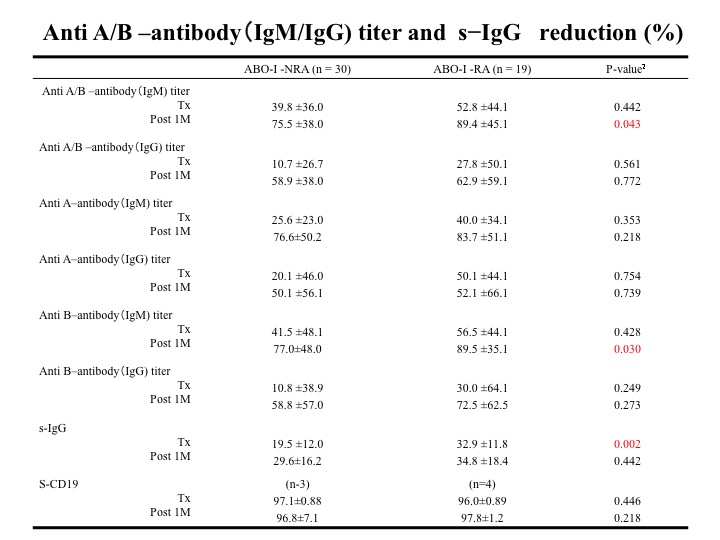
Conclusions: We realized that the most important point in our therapeutic strategy was the inhibition of antibody formation through pretransplant desensitization therapy.
Pretransplant desensitization therapy to suppress host B cell immunity against ABO-histo blood group antigens would be the most effective treatment to ensure the successful outcome of ABO-incompatible living-related kidney transplantation
