The Impact of Aorto-iliac Calcifications on Patient and Graft Survival in Renal Transplant Recipients using the TASCII Classification
A.A. Rijkse1, H.J.A.N. Kimenai1, M.A. van der Zijden2, J.I. Roodnat2, S. Ten Raa3, D.C. Bijdevaate4, J.N.M. IJzermans1, R.C. Minnee1.
1Department of Transplantation surgery, Erasmus Medical Center, Rotterdam, Netherlands; 2Department of Internal Medicine, Erasmus Medical Center, Rotterdam, Netherlands; 3Department of Vascular surgery, Erasmus Medical Center, Rotterdam, Netherlands; 4Department of Radiology, Erasmus Medical Center, Rotterdam, Netherlands
Introduction: Kidney transplantation is the therapy of choice in patients with end-stage renal disease. Aorto-iliac calcifications are a relative contra-indication for renal transplantation, even though the influence on patient and graft survival remains poorly explored. Aorto-iliac calcifications can be classified using the Trans Atlantic Inter-Society Consensus (TASC) II classification, which is based on the presence and extent of aorto-iliac stenotic lesions. The aim of this study is to assess the impact of aorto-iliac calcifications on patient and graft survival using the TASC II classification.
Methods: This retrospective single-center study included all kidney transplant recipients from 2000-2016 who had imaging-proven pre-transplantation aorto-iliac stenotic lesions. Patients were classified according to the TASC II classification if aorto-iliac stenotic lesions were present. All patients transplanted between 2007-2011 without aorto-iliac stenotic lesions were used as a control group. Primary endpoints were patient and graft survival. Cox regression analysis was used to evaluate risk factors for mortality and graft loss.
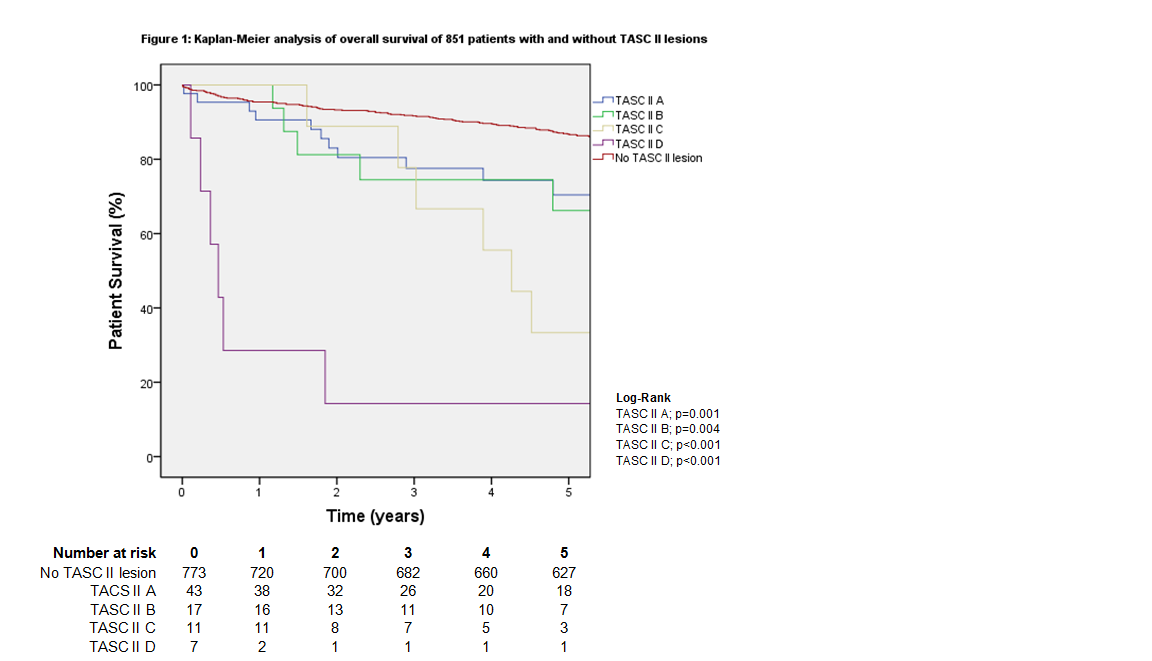
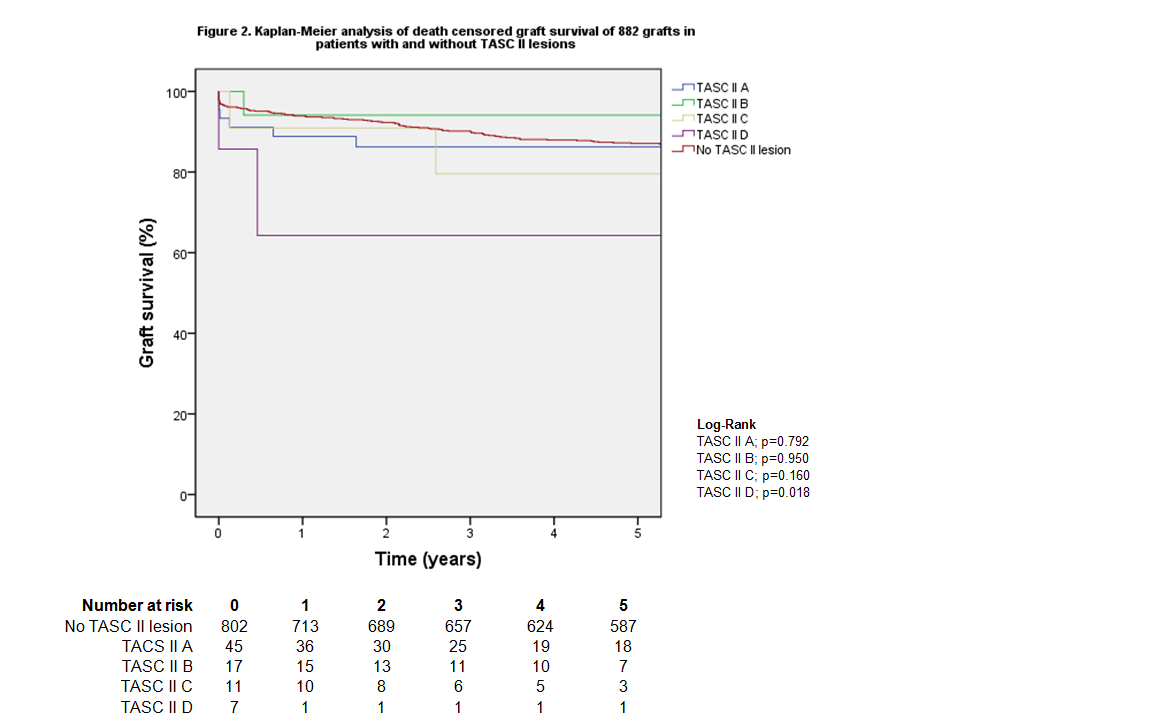
Results: Aorto-iliac stenotic lesions were observed in 78 patients before kidney transplantation. Seven hundred seventy-three patients were included as a control group. Overall patient survival was decreased for every TASC II class (TASC II A: p=0.001; B: p=0.004, C: p<0.001, D: p<0.001). No significant difference was found for 90-day mortality (TASC II A p=0.165; B p=1.000; C p=1.000) and 1-year mortality (TASC II A p=0.143; B p=1.000; C p=1.000) in patients with TASC II A, B or C lesions. Patients with TASC II D lesions had significantly higher 90-day (p=0.006) and 1-year (p <0.001) mortality. Death-censored graft survival was not significantly decreased for TASC II A, B and C compared to the control group (TASC II A p=0.792; B p=0.950; C p=0.160). Multivariate Cox model showed that any TASC II lesion was not a predictor of overall mortality (hazard ratio (HR) 1.52 confidence interval (CI) 0.94-2.46 p=0.091) or graft loss (HR 1.72; CI 0.94-3.17; p=0.080).
Discussion: This study demonstrates favorable outcomes in patients with TASC II A, B or C lesions with no increased mortality in the postoperative period. As expected, overall patient survival is decreased in patients with TASC II lesions because of cardiovascular comorbidity. The most striking result is similar death-censored graft survival in patients with TASC II A, B or C lesions and patients without any aorto-iliac stenotic lesions. Therefore, kidney transplantation in those patients is possible with favorable outcomes. The TASC II classification seems to be useful to predict patient outcomes.
Conclusion: Kidney transplantation is a safe procedure in patients with TASC II A, B and C lesions. Graft survival is unaffected by aorto-iliac stenotic lesions. Therefore, aorto-iliac calcifications should not be a contra-indication for kidney transplantation.