Kidney Allograft Histology in Recipients with Transplantation Vintage Longer than 10 Years
Tomoko Namba-Hamano1, Masahiro Kyo2, Takayuki Hamano3, Yutaka Yamaguchi4, Masataka Kawamura5, Shigeaki Nakazawa5, Taigo Kato5, Toyofumi Abe5, Ryoichi Imamura5, Naotsugu Ichimaru6, Shiro Takahara6, Norio Nonomura5, Yoshitaka Isaka1.
1Nephrology, Osaka University Graduate School of Medicine, Suita, Japan; 2Dialysis center, Sakurabashi Iseikai Clinic, Osaka, Japan; 3Comprehensive Kidney Disease Research, Osaka University Graduate School of Medicine, Suita, Japan; 4Pathology, Yamaguchi's Pathology Laboratory, Matsudo, Japan; 5Urology, Osaka University Graduate School of Medicine, Suita, Japan; 6Advanced Technology for Transplantation, Osaka University Graduate School of Medicine, Suita, Japan
Introduction and Aims: Kidney graft survival has improved dramatically during the recent several decades. However, few studies evaluated long-term graft histology. The aims of this study were to reveal the histological characteristics peculiar to long-term graft and to identify clinical manifestations associated with each histological finding.
Methods: In this retrospective study, we enrolled all allograft biopsies conducted in a single institution between 2002 and 2015 in recipients who had underwent transplantation 10 years before (88 biopsies).The revised Banff criteria were used to evaluate histological findings. We employed logistic regression analyses, to explore clinical factors associated with each histological parameter. Restricted cubic spline functions were used for non-linear associations.
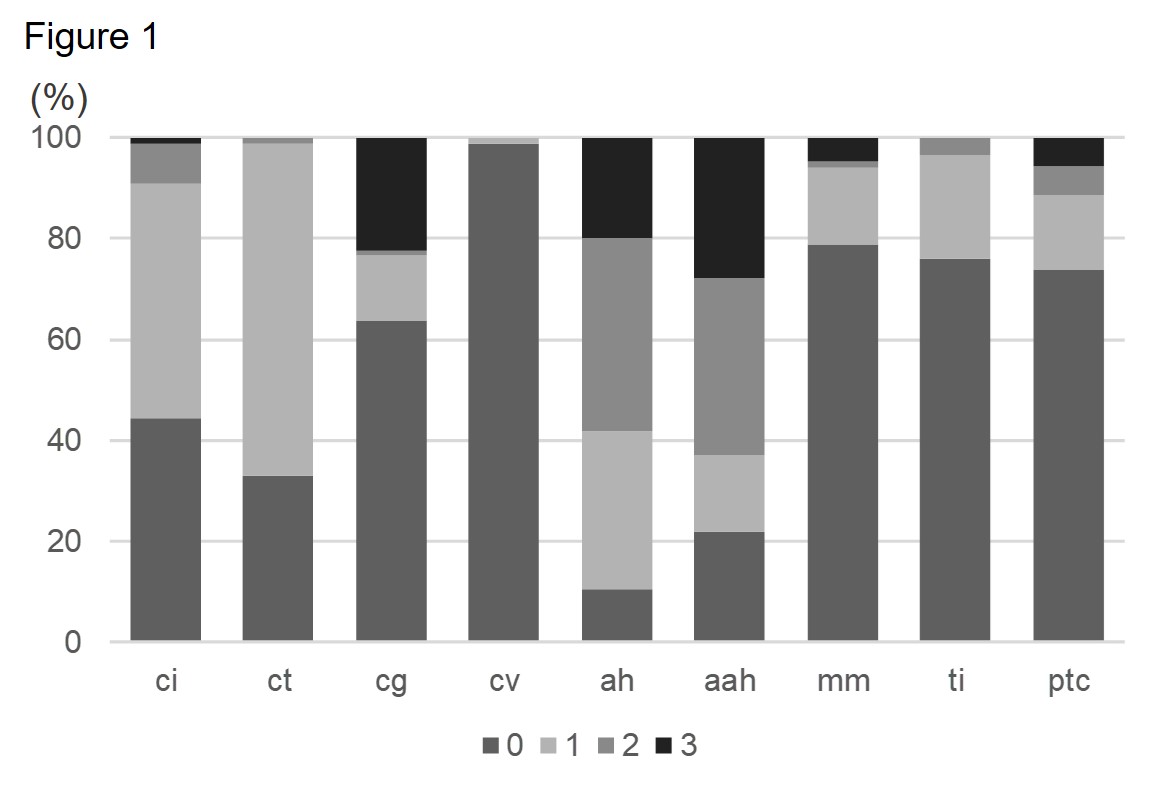
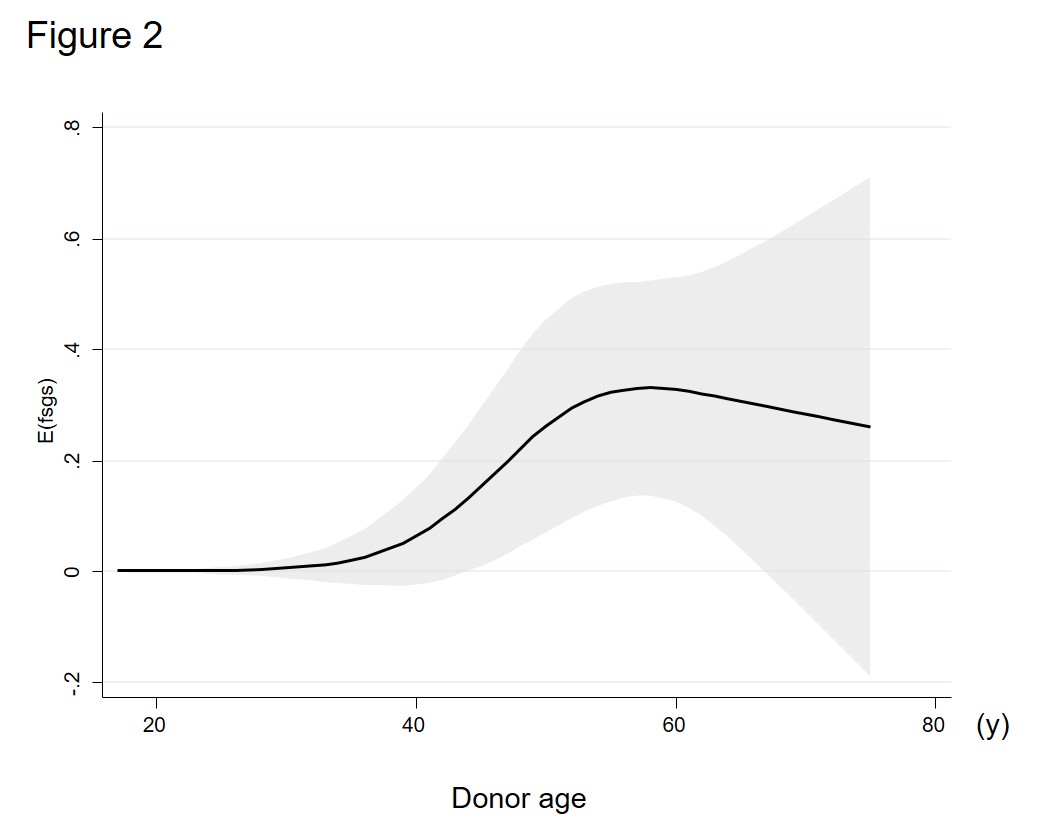
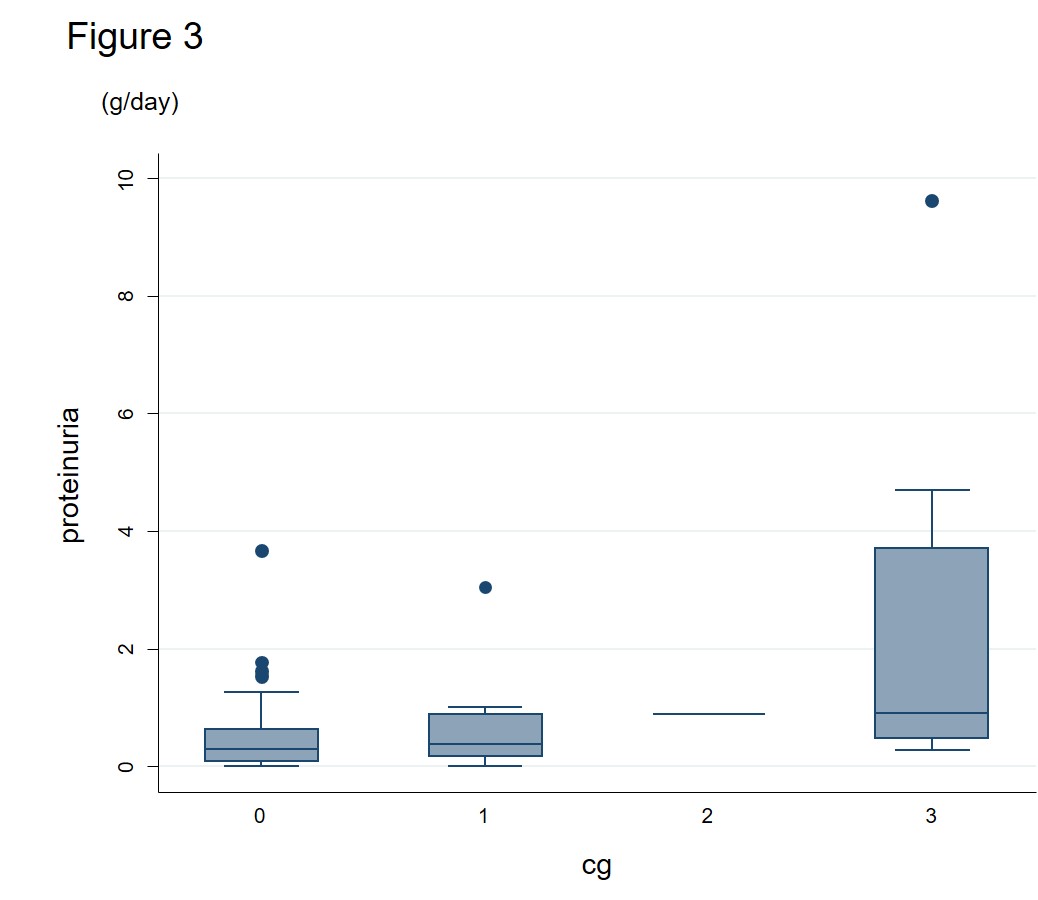
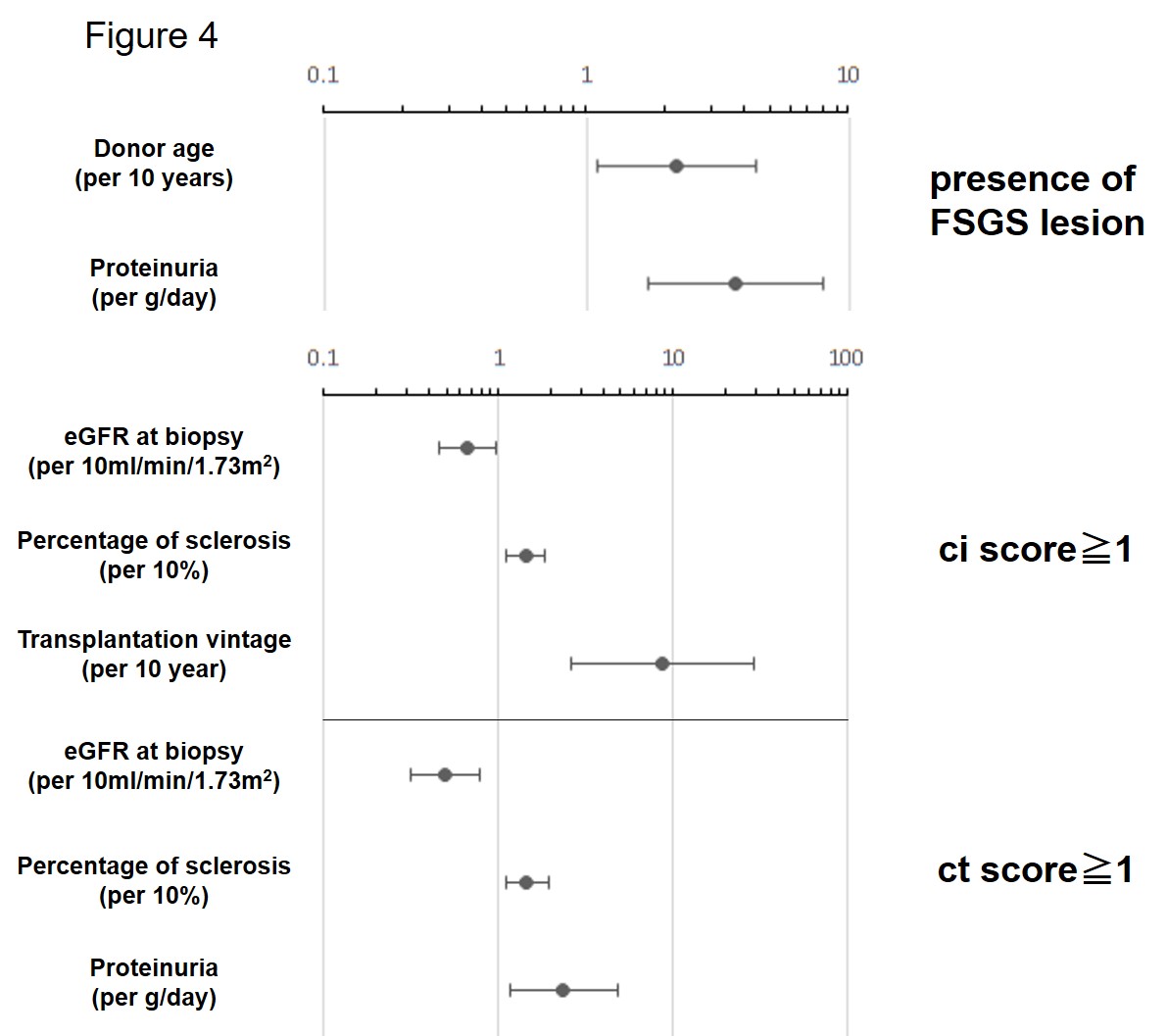
Results: Median (IQR) of time after transplantation, recipient age at biopsy, and donor age were 15 (11, 20), 50 (41, 60), and 50 years (41, 57), respectively. Only 21% were cadaveric transplantation. Median (IQR) eGFR and proteinuria at biopsy was 31(25,40) and 0.43(0.16,0.86), respectively. Indications for the biopsy were abrupt decrease in eGFR (39%), proteinuria (23%), relapse of glomerulonephritis (2%) and non-episode. Figure 1 shows the distribution of various histological parameters. Interstitial fibrosis and tubular atrophy were mild, if any, as ci and ct scores were dominantly grade1. Glomerular abnormalities were observed in 43%, such as FSGS-like lesion, crescent formation, mesangiolysis and transplant glomerulopathy. We confirmed that proteinuria was associated with the presence of FSGS lesion. Even after adjustment for proteinuria, donor age per 10 years was found to be associated with the presence of FSGS lesion [Odds ratio 2.19 (95%CI 1.10-2.19)]. When constructing a non-linear model, estimated prevalence of FSGS lesion was increased with aging of donors when older than 40 years old (Figure 2). Although the presence of transplant glomerulopathy (cg) was associated with FSGS lesion in a univariate analysis, adjustment for proteinuria extinguished this association. This is because high cg score was associated with greater proteinuria (Figure 3). Logistic regression analyses revealed that eGFR at biopsy, percentage of sclerotic glomorulus and transplantation vintage were associated with the presence of ci [Odds ratio 0.66 (95%CI 0.45-0.97),1.42 (1.11-1.82), and 8.72 (2.60-20.53), respectively]. We also found that eGFR at biopsy, percentage of sclerotic glomorulus and proteinuria were associated with the presence of ct [Odds ratio 0.50 (95%CI 0.32-0.78),1.45 (1.10-1.94), and 2.36 (1.16-4.80), respectively] (Figure 4).
Conclusions: Recipient’s eGFR reflects interstitial fibrosis and tubular atrophy. While transplantation vintage was associated with interstitial fibrosis, it was donor age that affects the prevalence of FSGS-like lesion in long-term graft.