Kidney Transplantation Utilising Donors After Circulatory Death – The First Report from the African Continent
Tinus Du Toit1, Kathryn Manning1, David Thomson1, Elmi Muller1.
1Department of Surgery , University of Cape Town, Cape Town, South Africa
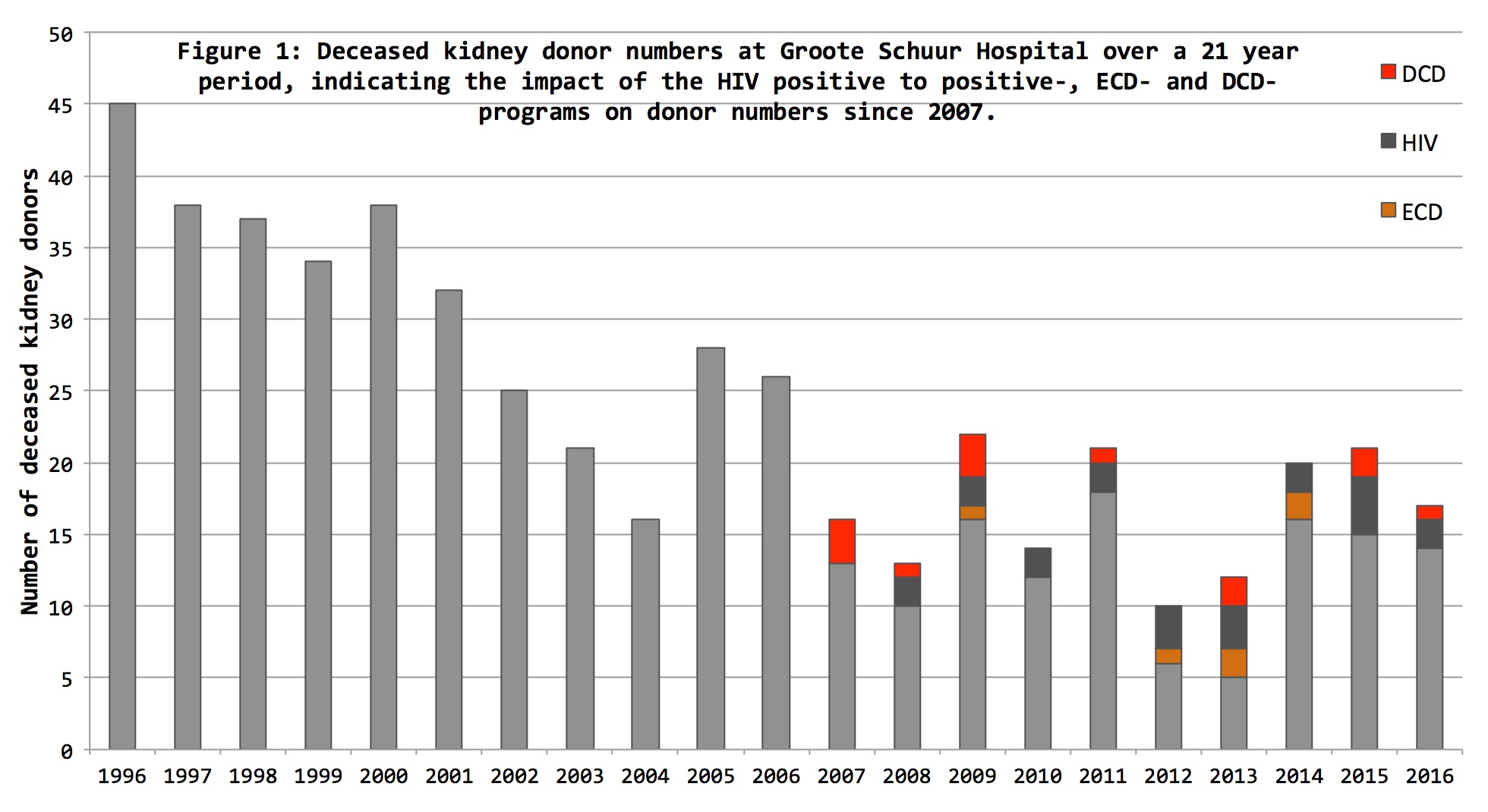
Introduction: At Groote Schuur Hospital, the number of deceased donors have declined over the last two decades, necessitating more liberal donor selection. In 2007, measures to expand the deceased kidney donor pool were implemented, including a HIV positive to positive transplant program, the utilisation of Extended Criteria Donors (ECD) as well as a Donation after Circulatory Death (DCD) program (Figure 1). Despite the successful implementation of DCD programs across Europe and the United Sates, other African centres have not adopted this mode of donation. The aim of this study was to report on our institutional experience with DCD kidney transplants and to encourage this approach among other African centres to improve access to transplantation.
Materials and methods: Retrospective, descriptive study of consecutive DCD renal transplants at Groote Schuur Hospital over a 10 year period (1 January 2007 to 31 December 2016). Data was obtained from donor referral and recipient registries. Primary end-points were defined as 1, 2 and 5 year graft- (censored for death with functioning graft) and patient survival. Kaplan-Meier method was used for survival analysis. Secondary end-points included the incidence of delayed graft function (DGF), 30-day morbidity, length of stay and donor and recipient clinical characteristics.
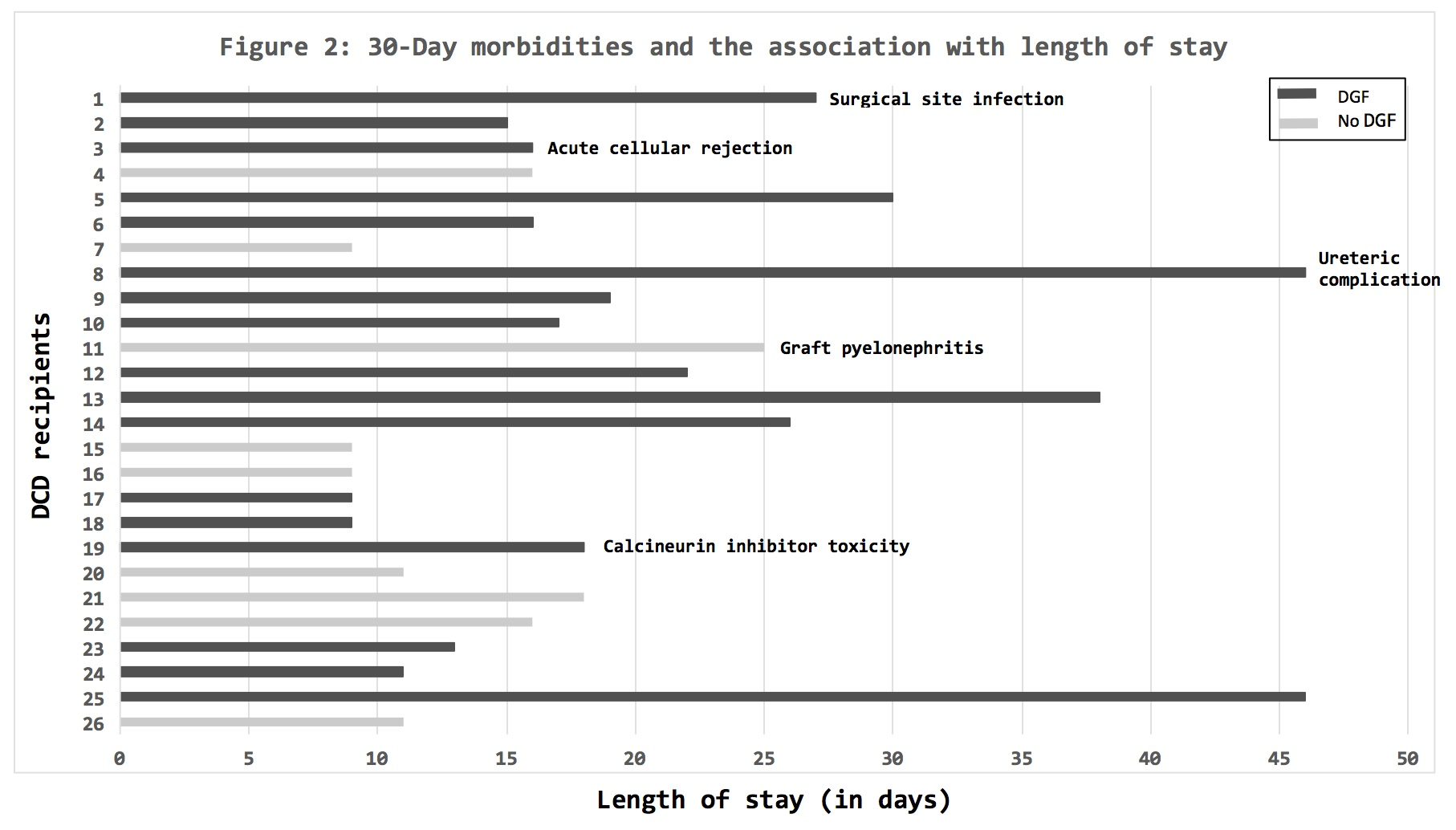
Results: 13 DCD procurements were performed, with no kidneys discarded. Utilised donors were young (median age 22 years; IQR 21-32) with well-preserved renal function (median terminal serum creatinine 86 umol/l; IQR 73-181). 26 Renal transplants were performed with a mean cold ischaemic time of 11 hours (IQR 8-14). Cumulative incidence of DGF was 65.4%. The median length of stay was 20 days (IQR 16-28) in those who experienced DGF and 11 days (IQR 9-16) in those who did not. 30-Day morbidity (other than DGF) was 19.2% (Figure 2). Graft survival at 1, 2 and 5 years were 100%, 95.8% (95% CI 73.9% - 99.4%) and 83.6% (95% CI 56.1%-94.8%) respectively (Figure 3). Patient survival at 1, 2 and 5 years was 92.3% (95% CI 72.6-98.0), as no deaths occurred between 1 and 5 years post-transplant (Figure 4).
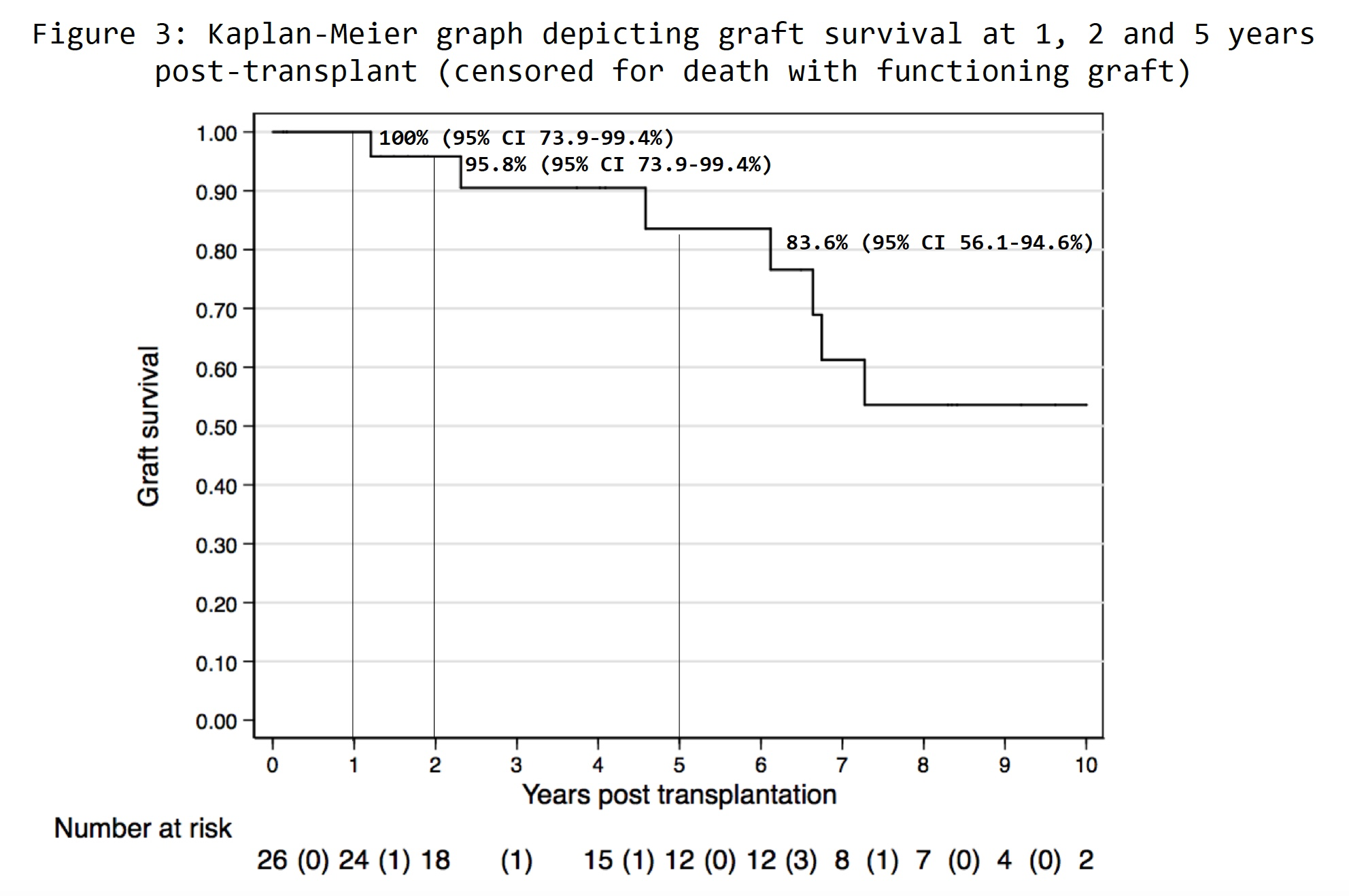
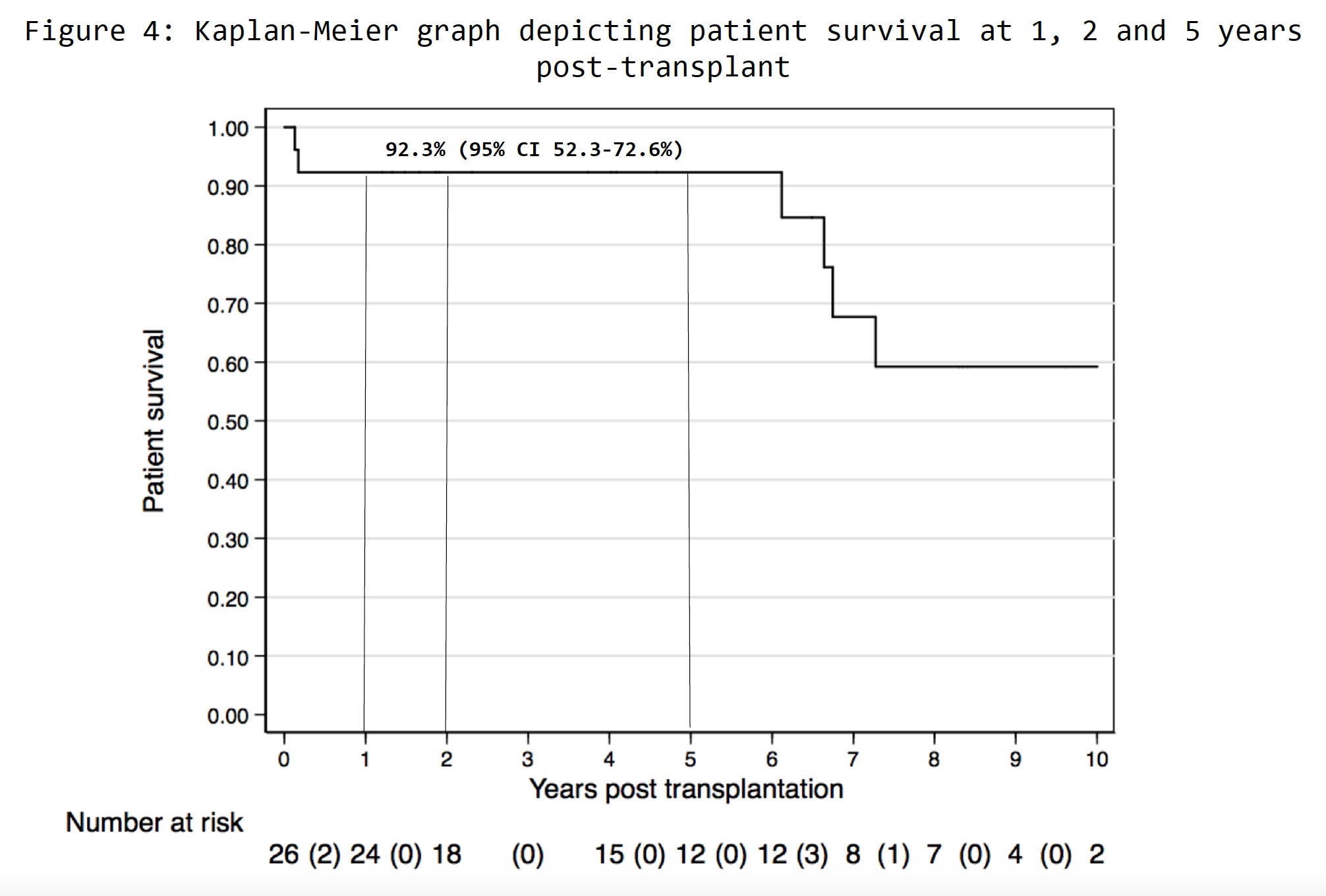
Discussion: Long term graft- and patient survival were comparable with international literature. The incidence of DGF was 65,4%. Possible explanations may include a high incidence of donor vasopressor requirements (46.2%), an initial learning curve with procurement technique and relatively long cold ischaemic times. Nevertheless, DCD may present an unique opportunity to expand deceased donation throughout Africa, particularly in areas hampered by a lack of brain death legislation and religious and/or cultural concerns regarding Donation after Brain Death.
Conclusion: Results from this study reaffirm the potential of DCD to expand deceased donation throughout Africa, in a religiously and culturally sensitive way.
