Intraoperative Renal Perfusion in Kidney Transplantation: A Retrospective Study.
Mauricio Sainz Barriga1, Maarten Naesens2, Nicholas Gilbo1, Ina Jochmans1, Diethard Monbaliu1, Dirk R. Kuypers2, Jacques Pirenne1.
1Department of Abdominal Transplantation Surgery, University Hospitals Leuven, KU Leuven, Leuven, Belgium; 2Department of Nephrology and Renal Transplantation, University Hospitals Leuven, KU Leuven, Leuven, Belgium
Aim: To explore whether intraoperative direct measurement of renal flows reflect ischemia/reperfusion injury and identify grafts at risk of inferior outcome in kidney transplantation, we conducted an observational retrospective single-center study.
Methods: Intraoperative direct transit-time flow measurements of renal artery flow (RAF) in mL/min were obtained immediately after graft reperfusion (M1) and prior to skin closure (M2). Patients were divided into the following 4 outcome groups: delayed graft function in patients requiring dialysis within postoperative day 7, non-dialysis requiring delayed graft function in patients with creatinine reduction ratio between postoperative days 1 to 2 (CRR2) ≤30%, immediate graft function (CRR2 >30%), and patients with vascular complications. Median and interquartile ranges are reported.
Results: 68 kidney transplants were included with a median follow-up of 12.6 (8.1-19.9) months. 16 living donors (LD), 35 donation after brain death donors (DBD) and 17 donation after cardiac death donors (DCD). Renal artery flow was available in 15 patients at M1 and in all 68 included patients at M2. An increase of flow between M1 and M2 was observed in 73% of cases.
Living donors showed significantly higher flows than deceased donors (table 1). 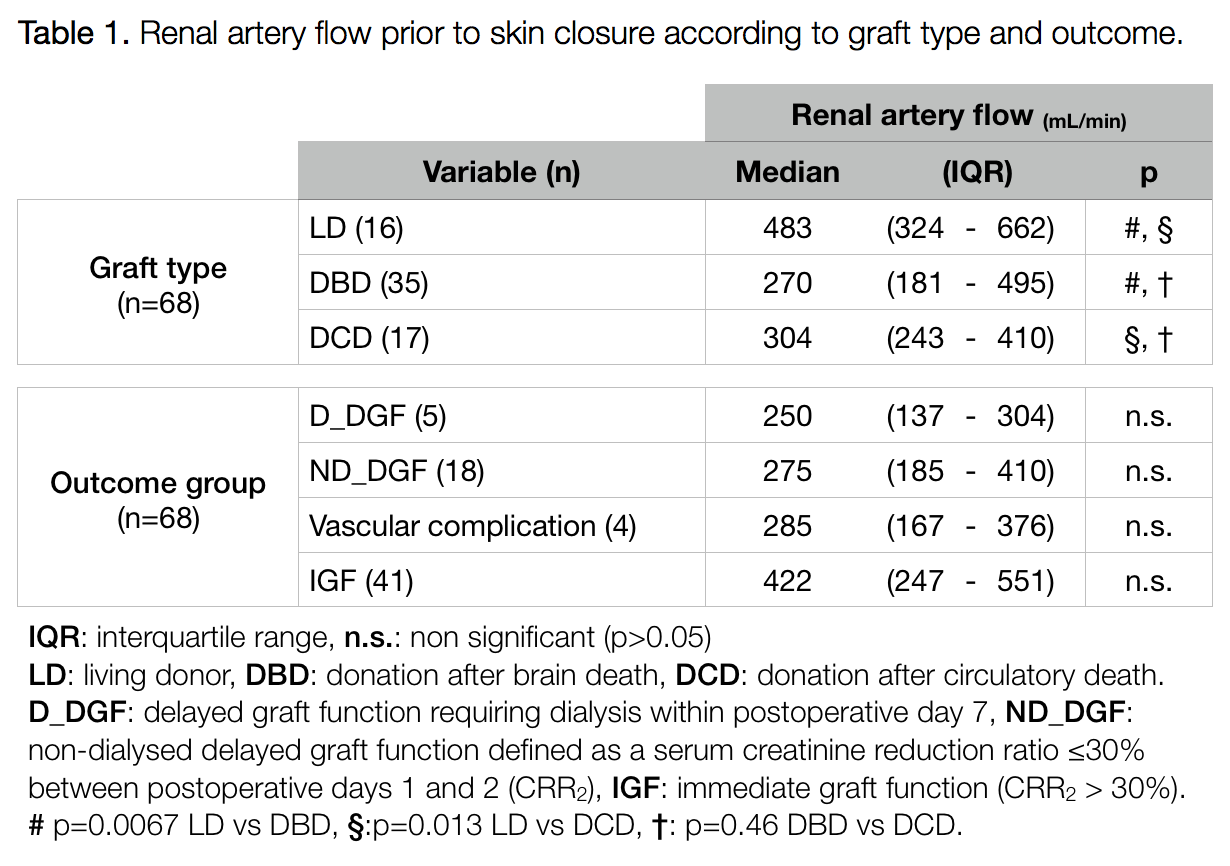 A creatinine reduction ratio between postoperative days 1 to 2 ≤30% was observed in all delayed graft function patients requiring dialysis or not and in 3 out of 4 vascular complication patients. Renal artery flow at M2 in these patients was significantly lower compared to immediate graft function patients: 259 (181-344) vs 419.5 (247-551), p=0.0065. Renal artery flow at M2 showed a negative correlation with recipient age (r=-0.28, p=0.002) but not with donor age (r=-0.23, p=0.058).
A creatinine reduction ratio between postoperative days 1 to 2 ≤30% was observed in all delayed graft function patients requiring dialysis or not and in 3 out of 4 vascular complication patients. Renal artery flow at M2 in these patients was significantly lower compared to immediate graft function patients: 259 (181-344) vs 419.5 (247-551), p=0.0065. Renal artery flow at M2 showed a negative correlation with recipient age (r=-0.28, p=0.002) but not with donor age (r=-0.23, p=0.058).
No PNF or irreversible rejection were observed. Graft loss occurred in 3 patients because of 2 renal artery thrombosis and 1 renal vein thrombosis in the early postoperative period. Normal curves with low flow or high resistance were observed at M1 with reduction of resistance at M2 (table 2). In 2 patients experiencing post-transplant arterial complications initial flows were normal or even high with a reduction of the flows at M2 (M2/M1 ≤1). The patient with postoperative renal vein thrombosis did not show any intraoperative findings in the arterial measurements.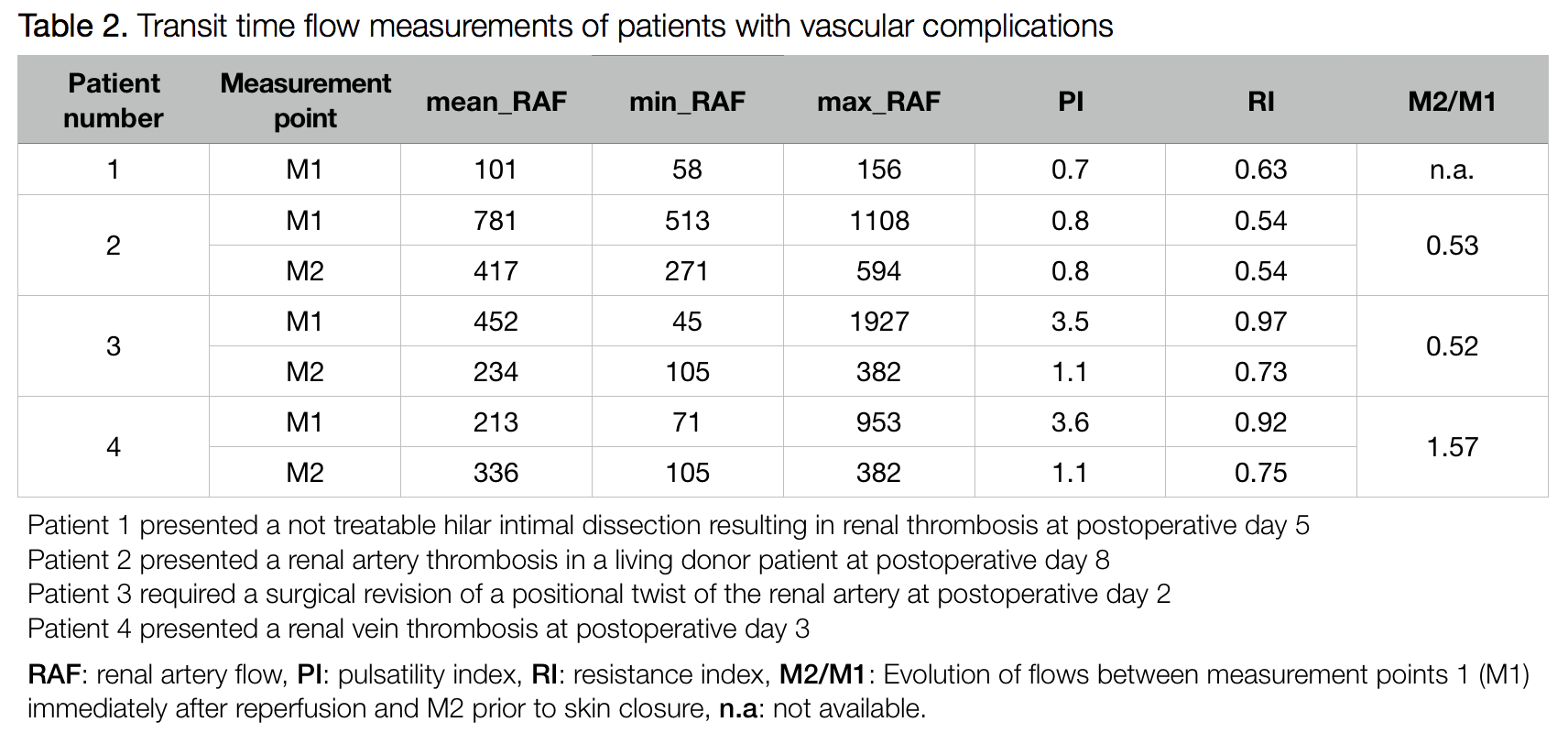
Conclusions: Our results demonstrates different flows according to graft quality. Patients receiving living donor grafts and with immediate graft function showed significantly higher intraoperative renal artery flows. Intraoperative direct renal artery flow measurement in kidney transplantation identified transplants at risk for worse outcome.
