Early Borderline Changes Represent a Risk for T-cell Mediated Rejection and Graft Failure in Kidney Transplantation
Petra Hruba1, Jana Maluskova2, Eva Honsova2, Janka Slatinska3, Mariana Wohlfahrtova3, Ondrej Viklicky1,3.
1Transplant laboratory, Centre for Experimental Medicine, Institute for Clinical and Experimental Medicine, Prague, Czech Republic; 2Department of Clinical and Transplant Pathology, Institute for Clinical and Experimental Medicine, Prague, Czech Republic; 3Department of Nephrology and Transplant Center, Institute for Clinical and Experimental Medicine, Prague, Czech Republic
Introduction: Borderline changes (BL) represent a frequent histological finding in kidney allograft with unclear outcome. Previously, we showed clear transcriptomic differences between early and protocol 3-months BL biopsies (Hruba et al. KI 2015). Therefore, the aim of our study was to compare the clinical outcome of early and subclinical 3-months BL in a large patient cohort.
Methods: BL were diagnosed in 781 out of 6197 kidney allograft biopsies (12.6%) performed from 2005 to January 2017. BL were mostly diagnosed in indication biopsies until 3-months (n=337, 43.1%), 35.9% (n=281) were found in 3-month protocol biopsies and 20.1% (n=163) in indication biopsies after 3-months. All BL cases were treated with methyprednisolone pulses (1-1.5g i.v.). Patients’ demographic, graft survival and Banff score of biopsies were compared between early indication (≤ 14 days after transplantation) (n=206) and 3-months protocol biopsies (n=198) with BL as a first pathology and between those who experienced or not later acute rejection. Continuous variables were compared by two-tailed Mann-Whitney and categorical variables using the chi-square test. For prediction of T-cell mediated rejection (TCMR) development, ROC curve analysis was used.
Results: Patients with subclinical BL in 3-months protocol biopsies had higher recipient age (51.7 vs 48.6 years; p=0.011), lower proportion of female donors (53.4% vs 42.3%; p=0.037), and received ATG induction treatment (34.8% vs 8.25%; p<0.001) compared to patients with early BL. Regarding Banff score, early BL group had higher i-score (p<0.001). Patients with early BL had worse 5 years graft survival than those with BL found in protocol biopsies (84.6% vs 93.3%, log rank p=0.018) (Fig.1). More patients after early BL developed TCMR (n=47 (22.8%)) compared to BL found in protocol biopsies (n=9 (4.5%); p<0.001). In order to find risk factors for TCMR development after early BL diagnosis, clinical characteristics and Banff scores between rejectors and nonrejectors were compared. While no differences in clinical characteristics were found, higher hyaline arteriolar thickening (aah) (p=0.010) and the incidence of mild glomerulitis (g1) (p=0.022) was present in those patients who progressed into TCMR. The prediction of TCMR using composite histological score (cv+aah+g1) had just marginal significance (receiver operating characteristic area under the curve for discriminating rejectors from nonrejectors was 0.63; cut-off>1.25 with sensitivity 61.4% and specificity 64.9%).
Conclusion: Contrary to 3-months protocol BL, patients with early BL are at risk of subsequent T-cell mediated rejection and graft failure within 5 years follow up. Therefore, early BL finding warrants intensive patients monitoring and modification of maintenance immunosuppression.
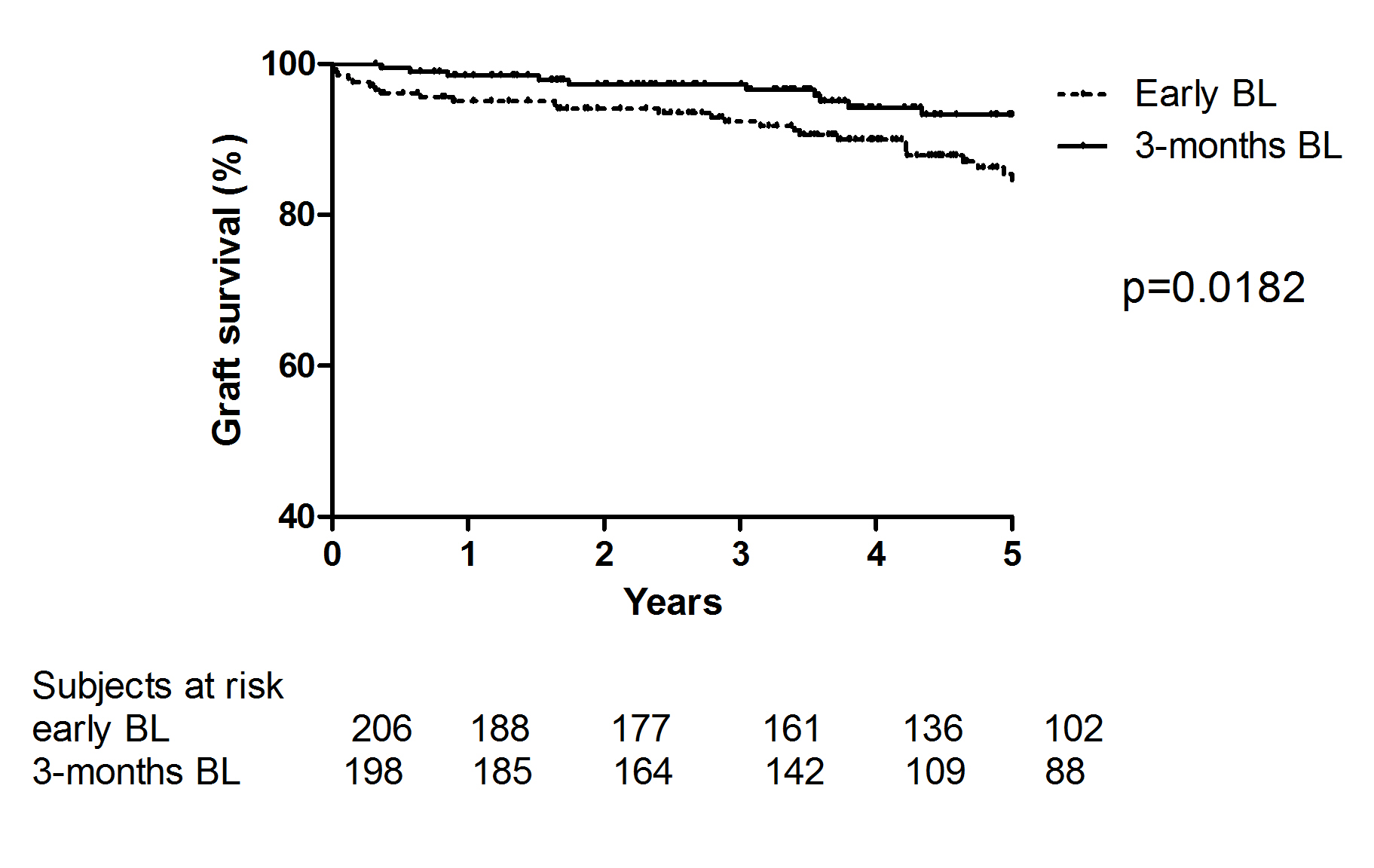
Fig.1 Graft survival of patients with early diagnosis of borderline changes (≤14 days after transplantation) compared to borderline changes diagnosed at 3-months protocol biopsies.
Supported by Ministry of Health of the Czech Republic (MZO 00023001) and by the Grant Agency of the Ministry of Health of the Czech Republic (17-28778A).
