Factors Associated with Time to Deceased Donor Renal Transplant Waitlisting or Living Donor Transplantation in Australia
Matthew P Sypek1,2,3, Philip A Clayton1,4,5, Wai Lim6,7, Peter Hughes2,3, John Kanellis8, Jenni Wright9, Jeremy Chapman10, Stephen P McDonald1,4,5.
1Australia and New Zealand Dialysis and Transplant Registry (ANZDATA), Adelaide, Australia; 2Dept of Medicine, Dentistry and Health Sciences, University of Melbourne, Melbourne, Australia; 3Dept of Nephrology, Royal Melbourne Hospital, Melbourne, Australia; 4Central and Northern Renal and Transplantation Services, Central Adelaide Local Health Network, Adelaide, Australia; 5Discipline of Medicine, University of Adelaide, Adelaide, Australia; 6Renal Department, Sir Charles Gairdner Hospital, Peter, Australia; 7School of Medicine and Pharmacy, University of Western Australia, Peter, Australia; 8Department of Nephrology, Monash Health and Centre for Inflammatory Disease, Monash University, Melbourne, Australia; 9National Organ Matching Service (NOMS), Australian Red Cross Blood Service, Sydney, Australia; 10Department of Renal Medicine, Westmead Hospital, Sydney Australia, Australia
Background: In order to be eligible for renal transplant waitlisting in Australia, a person must be receiving dialysis, have a low likelihood of perioperative mortality, and have an anticipated 80% likelihood of survival at five years post-transplantation. We aimed to provide the first detailed description of access to waitlisting or living donor (LD) renal transplantation in Australia, describe the characteristics of waitlisted patients and determine the patient factors associated with time to waitlisting or LD transplantation.
Methods: Data from the National Organ Matching Service and the Australia and New Zealand Dialysis and Transplant Registry were used to analyse access to transplantation (waitlisting for deceased donor transplant or LD transplant prior to listing) for all incident renal replacement therapy patients in Australia between July 2006-July 2015. Competing risk regression time to event models, with death as competing event, were used to determine predictors of waitlisting or LD transplantation.
Results: The cohort consisted of 21,290 patients with a median age of 63 years. At the completion of the follow up period 5,678 patients (26.7%) had been waitlisted or transplanted and 7,799 (36.6%) had died without being waitlisted or transplanted. By 2 years post commencing RRT, 69.3% of 18-24 year-old patients had been waitlisted or transplanted compared to 30.1% of 55-65 year-old patients and 8.0% of 65-75 year-old patients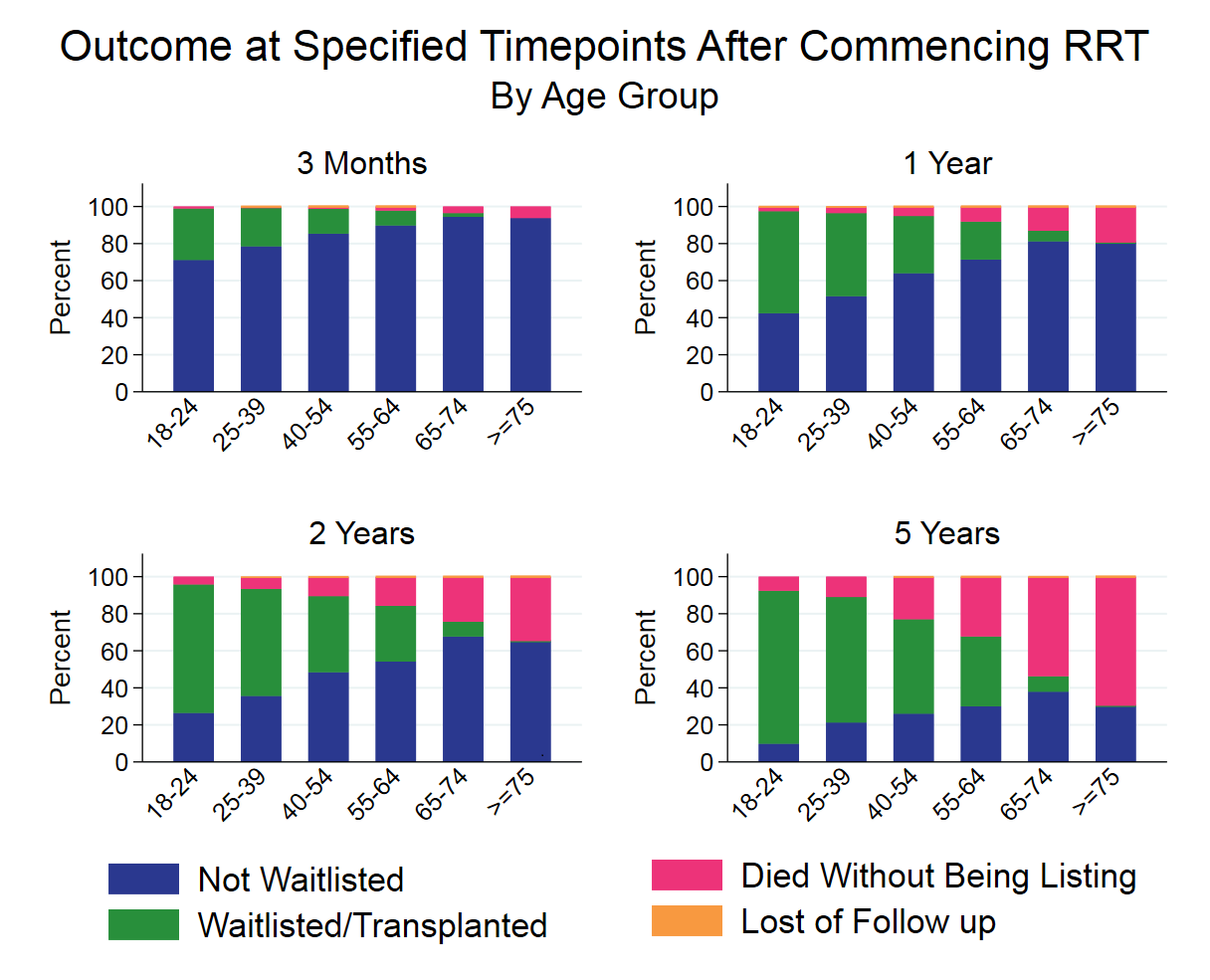 .
.
On multivariate regression all comorbidities included in the model were associated with a lower likelihood of waitlisting or LD transplantation, as was older age. There were considerable differences in access to transplantation across states. Indigenous patients were less likely to be waitlisted or transplanted compared to non-indigenous patients (SHR 0.35 [95%CI 0.30-0.42]) as were female patients compared to males (SHR 0.81 [95%CI 0.77-0.86]). Socio-economic disadvantage was associated with reduced access to transplantation. Both underweight and obese patients were less likely to be waitlisted or transplanted compared to patients in the normal BMI range (SHRs 0.75 [95%CI 0.64-0.88] and 0.68 [95%CI 0.63-0.73], respectively). The associations of smoking, history of cancer and late referral with waitlisting or transplantation were strongest in the period immediately after commencing RRT and diminished with time.
Conclusion: While it may be expected that factors related to poor post-transplant outcomes, such as comorbid conditions, would be associated with reduced likelihood of waitlisting or transplantation, our study highlights that a number of additional clinical, demographic, geographic and social factors are associated with access to transplantation in Australia. Further analysis is required to determine if this reflects appropriate implementation of current guidelines or highlights a need to address inequalities based on age, ethnicity, location of residence, gender, or socioeconomic disadvantage.
Australia and New Zealand Dialysis and Transplant Registry (ANZDATA). National Organ Matching Service (NOMS).
