Hepatitis C Virus Infected Kidney Wait List Patients: Treat with DAA or Delay?
Bryce Kiberd1, Karen Doucette2, Amanda Miller1, Karthik Tennankore1.
1Medicine, Dalhousie University, Halifax, NS, Canada; 2Medicine, University of Alberta, Edmonton, AB, Canada
Introduction: Currently many centers transplant HCV positive (+) donor kidneys into HCV+ recipients. Directed donation of HCV+ organs reduces the wait time to transplantation. Direct acting antiviral (DAA) therapy has the ability to cure HCV infection. Some have suggested that treatment of HCV+ wait listed patients be deferred with the hope that earlier transplantation will provide better outcomes than early DAA therapy. However there are not enough organs to guarantee prompt transplantation for the current wait list of infected candidates. If you are on the list is it better to wait or be treated early with DAA therapy?
Materials and Methods: A Markov medical decision analysis model was created to compare the overall outcomes of delay DAA therapy (Option 1) to immediate DAA therapy (Option 2) in wait listed HCV+ patients. Option 1 patients could receive either HCV+ or HCV- kidney and be treated at the time of transplantation, Option 2 would receive only HCV- organs. US mortality rates for adult wait-listed, functioning transplant and dialysis (failed transplant) cohorts and graft survival rates were used (baseline case age 50). The perspective was the patient, time horizon 50 years, and time 0 was wait listing date. DAA therapy resulted in cure. Relative mortality risk (RR) in HCV+ patients was 1.29 (1.11-1.79) compared to non-infected HCV- US patients. Treatment reduced RR of death by 65% (0.5-0.8).
Results and Discussion: Option 1 patients were modeled to be transplanted 1 year earlier with a higher cumulative transplant incidence (60% versus 54% for Option 2) (Figure 1). 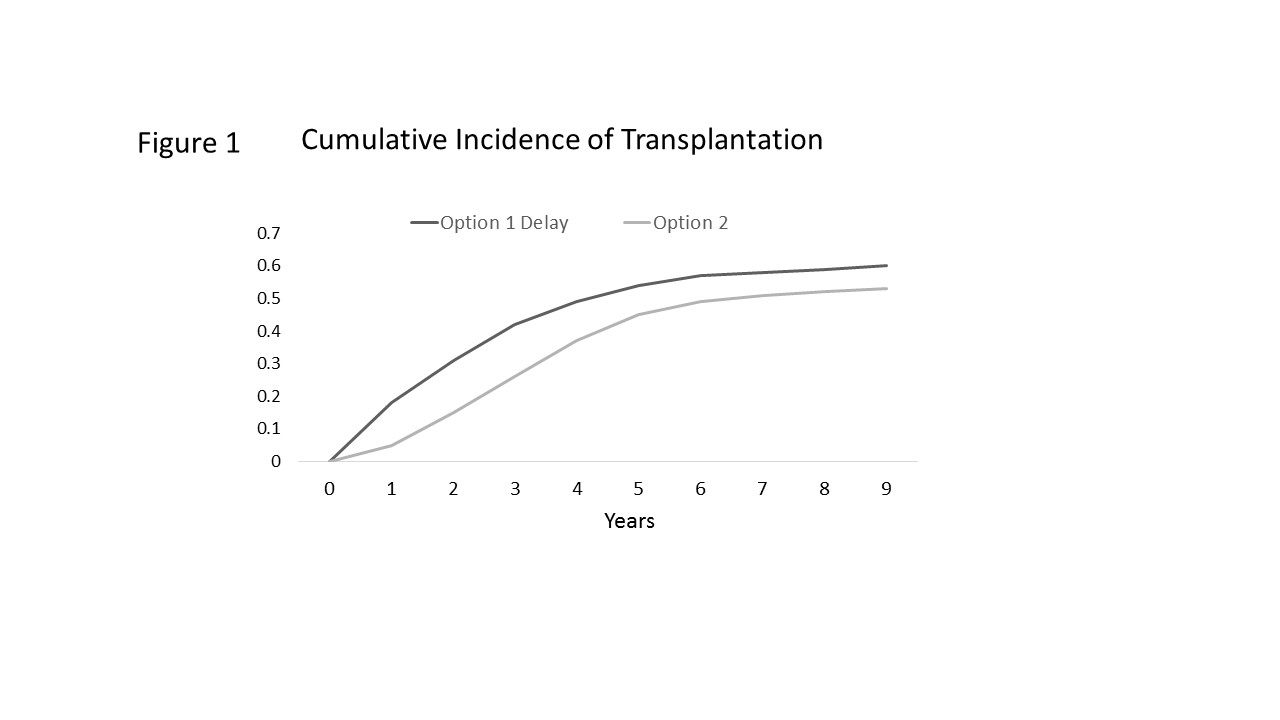 Despite this, Option 2 provided 0.43 (95% CI, 0.38, 0.49) more life years than Option 1. The Tornado plot (Figure 2) shows the differences between Option 1 and 2 for the key variables.
Despite this, Option 2 provided 0.43 (95% CI, 0.38, 0.49) more life years than Option 1. The Tornado plot (Figure 2) shows the differences between Option 1 and 2 for the key variables. 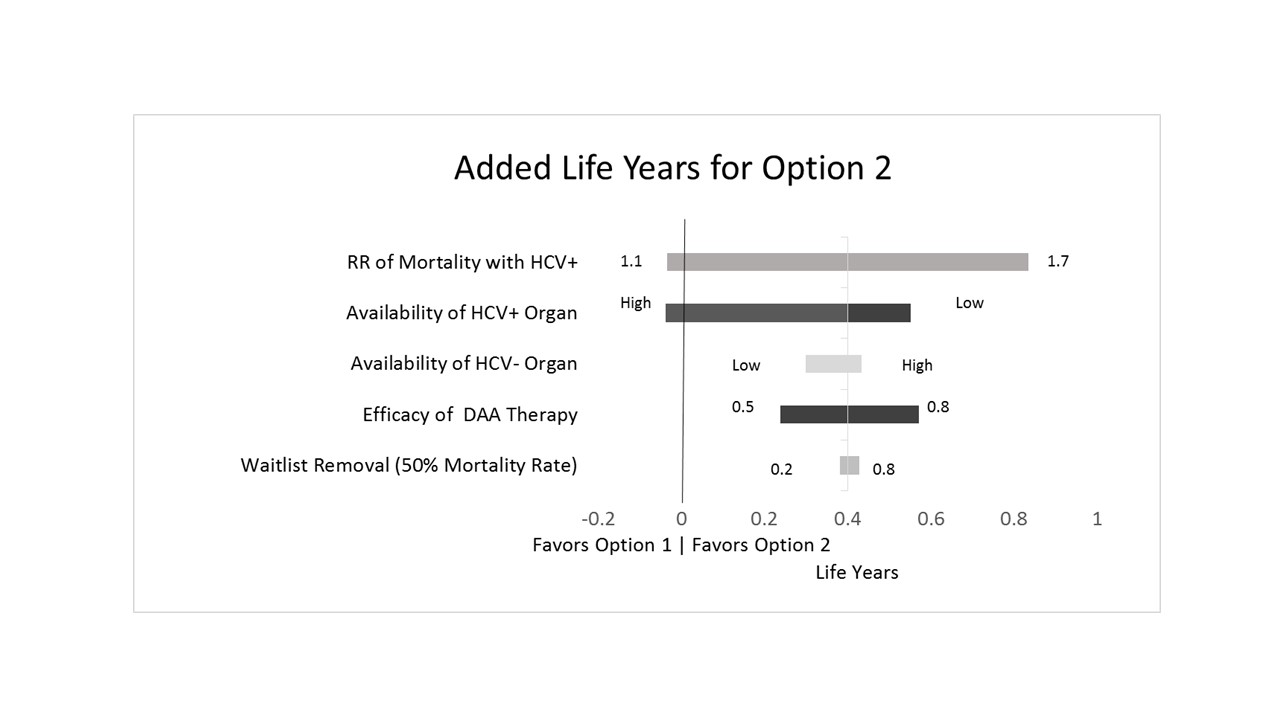 Over the range of most variables Option 2 provided more added (incremental) life years than Option 1, except in situations of a very low associated mortality with HCV infection and regions with much greater access to HCV+ organs (Figure 3).
Over the range of most variables Option 2 provided more added (incremental) life years than Option 1, except in situations of a very low associated mortality with HCV infection and regions with much greater access to HCV+ organs (Figure 3). 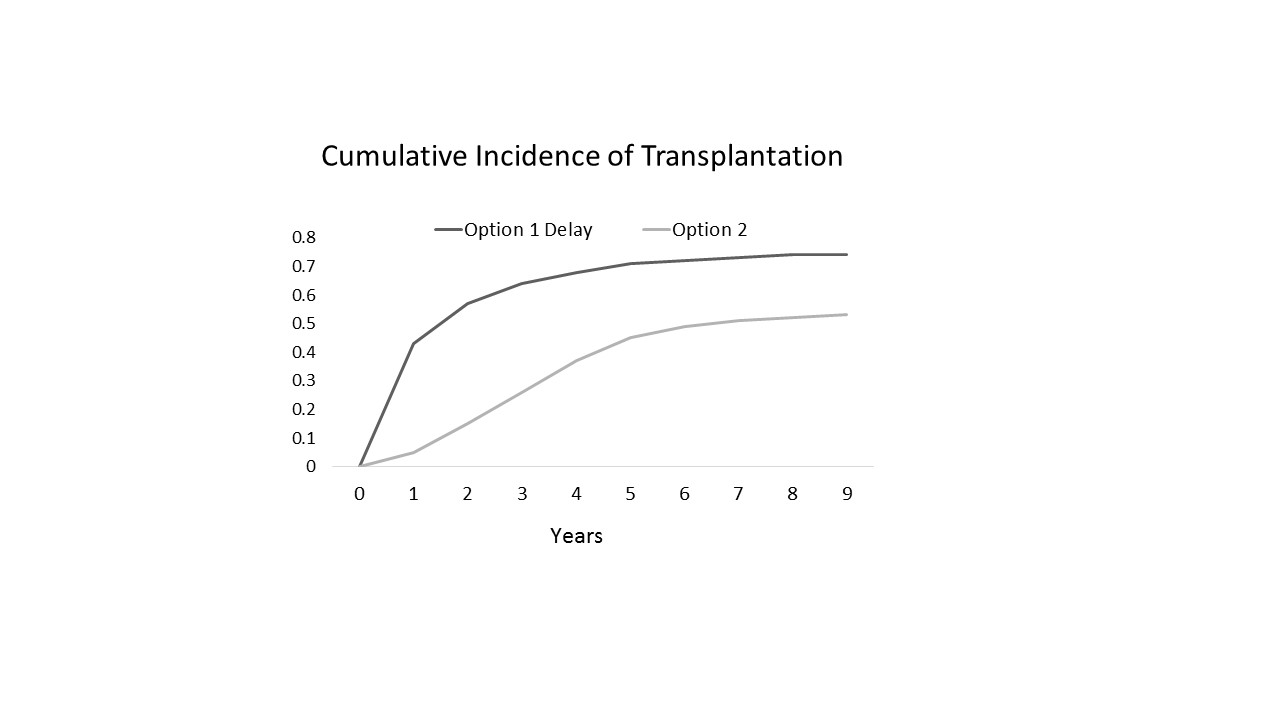 The findings were the same for younger (age 30) and older recipients (age 65). Including quality of life scores and calculating QALYS resulted in similar conclusions.
The findings were the same for younger (age 30) and older recipients (age 65). Including quality of life scores and calculating QALYS resulted in similar conclusions.
The best option from an individual patient’s perspective will differ by region and candidate. Early transplantation does not always overcome the excess risk of delayed HCV treatment. Early treatment with DAA should be considered in regions with relatively high demand (many on the wait list with HCV) but low supply of HCV+ organs or if there is a higher chance that delay will result in significant burden of disease associated mortality.
